|
 Symptoms
of malaria include fever and flu-like illness, including
shaking chills, headache, muscle aches, and tiredness. Nausea,
vomiting, and diarrhoea may also occur. Malaria may cause
anaemia and jaundice (yellow colouring of the skin and eyes)
because of the loss of red blood cells. Infection with one
type of malaria, P. falciparum, if not promptly treated, may
cause kidney failure, seizures, mental confusion, coma, and
death. Symptoms
of malaria include fever and flu-like illness, including
shaking chills, headache, muscle aches, and tiredness. Nausea,
vomiting, and diarrhoea may also occur. Malaria may cause
anaemia and jaundice (yellow colouring of the skin and eyes)
because of the loss of red blood cells. Infection with one
type of malaria, P. falciparum, if not promptly treated, may
cause kidney failure, seizures, mental confusion, coma, and
death.
For most people, symptoms begin 10 days to 4 weeks
after infection, although a person may feel ill as early as
8 days or up to 1 year later. Two kinds of malaria, P. vivax
and P. ovale, can relapse; some parasites can rest in the
liver for several months up to 4 years after a person is bitten
by an infected mosquito . When these parasites come out of
hibernation and begin invading red blood cells, the person
will become sick.
 Any
traveller who becomes ill with a fever or flu-like illness
while travelling and up to one year after returning home should
immediately seek professional medical care. You should tell
your GP that you have been travelling in a malaria-risk area. Any
traveller who becomes ill with a fever or flu-like illness
while travelling and up to one year after returning home should
immediately seek professional medical care. You should tell
your GP that you have been travelling in a malaria-risk area.
Malaria can be cured with prescription drugs. The type
of drugs and length of treatment depend on which kind of malaria
is diagnosed, where the patient was infected, the age of the
patient, and how severely ill the patient was at start of
treatment.
Anybody travelling to an area where malaria is endemic
is at risk of catching the disease. Lately there has been
an increase in the cases of malaria reported in the UK - in
1993 there were 1922 reported cases in the UK, including five
deaths. All caught the disease abroad and almost all cases
could have been prevented.
Be aware of the fact that adventure travellers
are usually more exposed to malaria than ordinary travellers
due
to the nature of their activities and the fact that they travel
to the more remote locations.
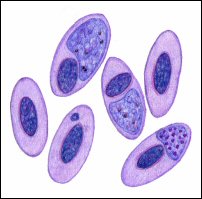
| The
Malaria Cycle (Plasmodium life cycle) |
|
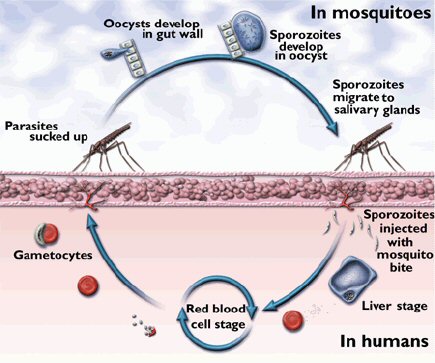 |
Ruptured
blood cells release free parasites (gametocytes) into
the host's bloodstream.
The human host shows the classic malaria symptoms at
this stage.
The gametocytes are sucked up by a feeding mosquito
and the cycle begins again.
|
The
Prevention and Treatment of Malaria
|
Malaria
is a preventable infection that can be fatal if left
untreated.
 You
cannot be vaccinated against malaria (yet), You
cannot be vaccinated against malaria (yet),
but you can protect yourself.
Click
on the image (right) to view a video presentation showing
the dangers of Malaria,
how easily it can spread, and it's effects on humans.
|
| Hope
for a new malaria vaccine |
|
 The
world's first malaria vaccine, has received a green
light for future use in babies in sub-Saharan Africa. The
world's first malaria vaccine, has received a green
light for future use in babies in sub-Saharan Africa.
The European Medicines Agency gave the Mosquirix vaccine
a favorable review after 30 years of research by the
Malaria Vaccine Initiative. The drug will now be examined
by the World Health Organization.
Individual countries will also need to give the vaccine
their final approval before it can be administered to
children.
The trials showed the vaccine was most effective in
newborn children between the ages of five and 17 months,
cutting the number of malaria cases by almost a half.
The number of cases in younger babies dropped by 27%.
Mosquirix is aimed at young children because
their immune system is still developing. There is currently
no vaccine available to travellers.
Unlike other vaccines that tackle viruses and bacteria,
Mosquirix has been designed to prevent illness caused
by a parasite. It works by stopping the malaria parasite
maturing and multiplying in the liver, after which it
would normally enter the patient's bloodstream and trigger
the disease symptoms.
The vaccine is given out in three doses one month apart,
with an additional booster dose a year and half later
to maintain protection.
Even though malaria is preventable and treatable, the
mosquito born disease killed 584,000 people in 2013,
with 90% of the deaths occurring in sub-Saharan Africa.
Of the victims, 83% were children under the age of five.
The World Health Organization lists malaria as the fifth
biggest killer in sub-Saharan Africa.
The vaccine is not yet licensed in countries where malaria
is endemic.
|
Avoidance of Bites
Mosquitoes cause much inconvenience
because of local reactions to the bites themselves and from
the infections they transmit. Mosquito bites spread other
diseases such as yellow fever, dengue fever and Japanese B
encephalitis.
 Mosquitoes
bite at any time of day but the
anopheles bites in the night with most activity at dawn and
dusk. If you are out at night wear long-sleeved clothing and
long trousers. Mosquitoes
bite at any time of day but the
anopheles bites in the night with most activity at dawn and
dusk. If you are out at night wear long-sleeved clothing and
long trousers.
Mosquitoes
may bite through thin clothing,
so spray an insecticide or repellent on them. Insect repellents
should also be used on exposed skin.
Spraying insecticides in
the room, burning pyrethroid coils and heating insecticide
impregnated tablets all help to control mosquitoes. If you
are sleeping in an unscreened room a mosquito net (which should
be impregnated with insecticide) is a sensible precaution.
If sleeping out of doors it is essential. Portable, lightweight
nets are available.
NOTE: Things like Garlic, Vitamin B and ultrasound
devices do not prevent mosquito bites.
Taking Anti-Malaria Tablets
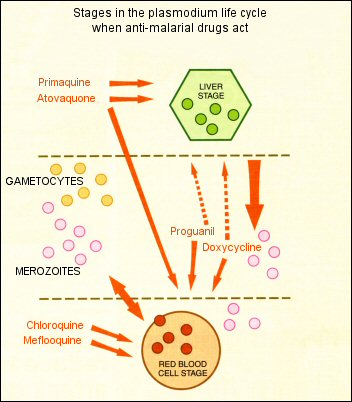
 It
should be noted that no prophylactic
regimen is 100% effective and advice on malaria prophylaxis
changes frequently. There are currently five prophylactic
regimens used (A,B,C,D & E), due to the differing resistance
that exists by the malaria parasites to the various drugs
used. (See the above map of Malaria Endemic Areas). It
should be noted that no prophylactic
regimen is 100% effective and advice on malaria prophylaxis
changes frequently. There are currently five prophylactic
regimens used (A,B,C,D & E), due to the differing resistance
that exists by the malaria parasites to the various drugs
used. (See the above map of Malaria Endemic Areas).
The tablets you require
depend on the country to which you are travelling (see the
table page). Start taking the tablets before travel take them
absolutely regularly during your stay, preferably with or
after a meal and continue to take them after you have returned.
This is extremely important to cover the incubation period
of the disease.
Prompt Treatment
If you
develop a fever between one week after first exposure
and up to two years after your return, you should seek medical
attention and inform the doctor that you have been in a malarious
area.
 Anyone
with suspected malaria should be treated under medical
supervision as soon as possible. If malaria is diagnosed then
treatment is a matter of urgency. Treatment should not normally
be carried out by unqualified persons. Anyone
with suspected malaria should be treated under medical
supervision as soon as possible. If malaria is diagnosed then
treatment is a matter of urgency. Treatment should not normally
be carried out by unqualified persons.
The drug treatment of malaria depends on the type and
severity of the attack. Typically, Quinine Sulphate tablets
are used and the normal adult dosage is 600mg every twelve
hours which can also be given by intravenous infusion if the
illness is severe.
Remember: Prevention
is better than cure and over two million people die from malaria
every year. It is a very serious illness!

Side Effects of Anti-Malarials
Like all medicines,
anti-malarials can sometimes cause side-effects:
Proguanil (Paludrine)
can cause nausea and simple mouth ulcers.
Chloroquine (Nivaquine
or Avloclor) can cause nausea, temporary blurred vision and
rashes.
 Patients
with a history of psychiatric disturbances (including
depression) should not take mefloquine as it may precipitate
these conditions. It is now advised that mefloquine be started
two and a half weeks before travel. Patients
with a history of psychiatric disturbances (including
depression) should not take mefloquine as it may precipitate
these conditions. It is now advised that mefloquine be started
two and a half weeks before travel.
Doxycycline does carry
some risk of photosensitisation i.e. can make you prone to
sunburn.
Malarone is a relatively
new treatment and is virtually free of side effects. It is
licensed for use in stays of up to 28 days but there is now
experience of it being taken safely for up to three months.
No other tablets
are required with mefloquine or doxycycline or Malarone.
 Drug
Resistance Drug
Resistance
It is the plasmodia that cause malaria that develop resistance
to anti-malarial drugs not the mosquitoes that transmit the
disease.
Resistance to antimalarial drugs is proving to be a challenging
problem in malaria control in most parts of the world. Since
the early 60s the sensitivity of the parasites to chloroquine,
the best and most widely used drug for treating malaria, has
been on the decline.
Drug resistance is the ability of a parasite species to survive
and multiply despite the administration of a drug in doses
equal to or higher than those usually recommended but within
the limit of tolerance.
 Newer
antimalarials have been developed in an effort to tackle this
problem, but all these drugs are either expensive or have
undesirable side effects. Newer
antimalarials have been developed in an effort to tackle this
problem, but all these drugs are either expensive or have
undesirable side effects.
The discovery of chloroquine revolutionalised the treatment
of malaria, pushing quinine to the sidelines.
However, after a variable length of time, the parasites, especially
the falciparum species, have started showing resistance to
these new drugs.
Resistance is most commonly seen in P. falciparum whereas
only sporadic cases of resistance have been reported in P.
vivax malaria.
Resistance to chloroquine is most prevalent, while resistance
to most other antimalarials has also been reported.
Resistance to chloroquine began from two epi-centres; Colombia
(South America) and Thailand (South East Asia) in the early
1960s. Since then, resistance has been spreading world wide.
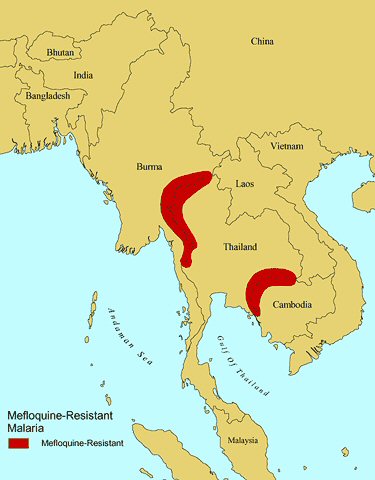
Recently, cases of mefloquine
resistance have been reported from areas of Thailand bordering
with Burma and Cambodia (see map left). Travellers to Thailand
are therefore advised to avoid using mefloquine when travelling
to these risk areas.
 Because
mefloquine is structurally similar to chloroquine, cross resistance
is possible Because
mefloquine is structurally similar to chloroquine, cross resistance
is possible
due to the prolonged half life of mefloquine.
Further
in-depth information about the malaria risk to travellers
can be obtained from the following documents (pdf format):-
|
The information supplied
here is derived from a number of reliable sources
and is compared and compiled into the alphabetical lists
found on this web site.
Countries requiring malaria prophylaxis should be
regarded as being at risk all year round and
you should also assume that the whole country
is at risk unless otherwise indicated. The malaria
regimen is the recommended regimen for a country.
Use of the incorrect regimen may not provide adequate
cover.
When there are two different regimens
for the same country, they are area specific. Read the
text to find out which regimen is suitable for the area
you require.
Where regimen 1 is indicated there is Chloroquine
resistance in that region and it is very likely to be
the Falciparum malaria which is the most serious form
of the disease. In this instance it is vitally important
that travellers take adequate prophylaxis.
Remember:- No prophylaxis is 100% effective
but not taking anti-malarials where they are indicated
will put you at greater risk should you get the disease.
Remember - Malaria is a killer!
|
|
The Different Drug Regimens
|
| Regimen
1 |
Mefloquine one 250mg tablet
weekly. OR
Doxycycline one 100mg capsule daily. OR
Malarone one tablet daily. |
| Regimen
2 |
Chloroquine 300mg
weekly (2x150mg tablets). PLUS
Proguanil 200mg daily (2x100mg tablets). |
| Regimen
3 |
Chloroquine 300mg
weekly (2x150mg tablets) OR
Proguanil 200mg daily (2x100mg tablets).
|
| Regimen
4 |
No
prophylactic tablets required but anti mosquito measures
should be strictly observed: Avoid
mosquito bites by covering up with clothing such as long
sleeves and long trousers especially after sunset, using
insect repellents on exposed skin and, when necessary,
sleeping under a mosquito net. |
| . |
| Proguanil
|
100mg tablets are
supplied as Paludrine Tablets |
| Chloroquine |
150mg tablets are
supplied as Nivaquine or Avloclor Tablets |
| Mefloquine
|
250mg tablets are
supplied as Lariam Tablets |
| Malarone |
is a
combination of Atovaquone 250mg and Proguanil
100mg |
|
Long Term
Use of Anti-Malaria Drugs
|
| Chloroquine |
May be
taken for periods exceeding five years. |
| Paludrine |
May be
taken for periods exceeding five years. |
| Maloprim |
Can be
taken for periods up to one year. |
| Mefloquine |
Can be
taken for periods up to one year. |
| Doxycycline |
Can be
taken for periods up to six months. |
| Malarone |
Can be
used for travel periods up to one year. |
|
Childrens' Dosages:
Calculate
the dose by weight rather than by age if possible
|
|
Age/Weight
|
Chloroquine
(once weekly)
|
Proguanil
(once daily)
|
Mefloquine
(once weekly)
|
Doxycycline
(once daily)
|
Malarone
(once daily)
|
|
0
- 12 weeks
under 6kg
|
1/4
tablet
|
1/4
tablet
|
-
|
-
|
-
|
|
3
- 12 months
6 - 10kg
|
1/2
tablet
|
1/2
tablet
|
1/4
tablet
|
-
|
-
|
|
1
- 3 years
10 - 16kg
|
3/4
tablet
|
3/4
tablet
|
1/4
tablet
|
-
|
1
child's
tablet
|
|
4
- 7 years
16 - 25kg
|
1
tablet
|
1
tablet
|
1/2
tablet
|
-
|
1
child's
tablet
|
|
8
- 12 years
25 - 45 Kg
|
11/2
tablets
|
11/2
tablets
|
3/4
tablet
|
-
|
2
child's
tablets
|
|
13
years and over
45kg and over
|
2
tablets
|
2
tablets
|
1
tablet
|
1
capsule
|
1
adult
tablet
|
|
The
above dosages are based upon the guidelines issued by
the Advisory Committee on Malaria Prevention.
|
|
Childrens' Dosages:
Calculate
the dose by weight rather than by age if possible
|
|
Age/Weight
|
Chloroquine
(once weekly)
|
Proguanil
(once daily)
|
Mefloquine
(once weekly)
|
Doxycycline
(once daily)
|
Malarone
(once daily)
|
|
0
- 12 weeks
under 6kg
|
1/4
tablet
|
1/4
tablet
|
-
|
-
|
-
|
|
3
- 12 months
6 - 10kg
|
1/2
tablet
|
1/2
tablet
|
1/4
tablet
|
-
|
-
|
|
1
- 3 years
10 - 16kg
|
3/4
tablet
|
3/4
tablet
|
1/4
tablet
|
-
|
1
child's
tablet
|
|
4
- 7 years
16 - 25kg
|
1
tablet
|
1
tablet
|
1/2
tablet
|
-
|
1
child's
tablet
|
|
8
- 12 years
25 - 45 Kg
|
11/2
tablets
|
11/2
tablets
|
3/4
tablet
|
-
|
2
child's
tablets
|
|
13
years and over
45kg and over
|
2
tablets
|
2
tablets
|
1
tablet
|
1
capsule
|
1
adult
tablet
|
|
The
above dosages are based upon the guidelines issued by
the Advisory Committee on Malaria Prevention.
|
|
Adult
Dosages
|
|
Regimen
|
Dose
for
Chemoprophylaxis
|
Usual
amount
per tablet (mg)
|
| Areas
without drug resistance: |
|
Chloroquine
Proguanil
|
2
tablets weekly
2
tablets daily
|
150mg
(base)
100mg
|
| Areas
of little chloroquine resistance (poorly effective where
marked resistance): |
Chloroquine
plus
Proguanil |
2
tablets weekly
2 tablets daily |
150mg
(base)
100mg |
| Areas
of chloroquine resistant P. falciparum: |
|
Mefloquine
Doxycycline
Malarone
(atovaquone & proguanil)
|
1
tablet weekly
1
tablet/capsule daily
1
tablet daily
|
250mg
(228 in USA)
100mg
250mg
atovaquone &
100mg proguanil
|
| Countries
where there is currently no risk of malaria: |
|
|
| Malaria
prophylaxis for Sub-Saharan Africa |
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
| Low
risk |
- Cape
Verde - Remember, low risk if fever develops.
- Mauritius
- Except a few rural areas where chloroquine prophylaxis
is appropriate.
|
Avoid
insect bites. |
|
| Risk
in parts of the country Some chloroquine resistance present.
|
- Botswana
- Only in the northern half of the country - November
to June.
- Mauritania
- All year round in the south. November to June in
the north.
- Zimbabwe
- Areas below 1,200 metres - November to June. All
year long in the Zambezi Valley where Doxycycline,
Mefloquine or Malarone are preferable. Risk is negligible
in Harare and Bulawayo.
|
Chloroquine
PLUS
Proguanil |
Doxycycline
OR
Mefloquine
OR
Malarone |
| Risk
very high, or locally very high. Chloroquine resistance
very widespread. |
- Angola
- Benin
- Burkina
Faso
- Burundi
- Cameroon
- Central
African Republic
- Chad
-
Comoros
- Congo
- Djibouti
- Equatorial
Guinea
- Eritrea
|
- Gabon
- Gambia
- Ghana
- Guinea
- Guinea
Bissau
- Ivory
Coast
- Kenya
- Liberia
- Madagascar
- Malawi
- Mali
- Mozambique
- Niger
- Nigeria
|
- Principe
- Rwanda
- Sao
Tome
- Senegal
- Sierra
Leone
- Somalia
- Sudan
- Swaziland
- Tanzania
- Togo
- Uganda
- Zaire
- Zambia
|
- Ethiopia
- Areas below 2,200 metres. No risk in Addis Ababa
- Namibia
- The northern third of the country - November to
June. All year long around the Kavango and Kunene
rivers.
- South
Africa - North east, low altitude areas of Mpumalanga
and Northern Provinces, Northeast KwaZulu-Natal as
far south as the Tugela river. Risk present in Kruger
National Park.
- Zimbabwe
- The Zambezi Valley.
|
Doxycycline
OR
Mefloquine
OR
Malarone
|
Chloroquine
PLUS
Proguanil - (limited protection)
|
| Malaria
prophylaxis for North Africa, Middle East & South
West Asia |
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
| Risk
very low. |
- Algeria
- Virtually no risk
- Egypt
- Main tourist areas are malaria free.
- Georgia
- Some south eastern villages July to October.
- Kyrgystan
- Some southern and western areas.
- Libya
- Morocco
- A few rural areas only limited risk.
- Turkey
- Most tourist areas.
- Uzbekistan
- Sporadic cases in extreme south east only.
|
Avoid
mosquito bites |
|
| Risk
low |
- Armenia
- The whole country June to October.
- Azerbaijan
- Southern border area June to October.
- Egypt
- El Faiyum region only, June to October.
- Iraq
- Basrah and rural north, May to November.
- Syria
- Northern border, May to October.
- Turkey
The plain around Adana, Side & south east Anatolia,
March to November.
- Turkmenistan
- The south east only, June to October.
|
Chloroquine |
Proguanil |
| Risk
present. Some chloroquine resistance present. |
- Afghanistan
- Areas below 2,000 metres, May to November.
- Iran
- Oman
- Remote rural areas only.
- Saudi
Arabia - The whole country except northern, eastern
and central provinces, Asir plateau, and western border
cities where there is very little risk. No risk in
Mecca.
- Tajikistan
- Southern border areas, June to October.
- Yemen
- No risk in Sana'a city.
|
Chloroquine
PLUS
Proguanil |
|
| Malaria
prophylaxis for South Asia (Indian Subcontinent)
|
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
| Very
low risk. |
- Maldives
- no risk
- India
- No risk in parts of mountain states of the north.
|
Avoid
mosquito bites |
|
| Risk
variable. Chloroquine resistance usually moderate. |
- Bangladesh
- The whole country except Chittagong Hill Tracts.
No risk in Dhaka City.
- Bhutan
- Southern districts only.
- India
- All areas below 2,000 metres, including Goa.
- Nepal
- Areas below 1,500 metres, especially Terai districts.
No risk in Kathmandu.
- Pakistan
- Areas below 2,000 metres.
- Sri
Lanka - No risk in Colombo.
|
Chloroquine
PLUS
Proguanil |
Will
vary locally. |
Risk
high.
Chloroquine resistance high. |
- Bangladesh
- Chittagong Hill Tract Districts only.
- India
- Assam region.
|
Doxycycline
OR
Mefloquine
OR
Malarone
|
Chloroquine
PLUS
Proguanil |
| Malaria
prophylaxis for South East Asia |
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
| Risk
very low. Remember malaria is possible if fever develops. |
- Bali
- Part of Indonesia
- China
- Main tourist areas.
- Hong
Kong
- Indonesia
- Jakarta, main cites and tourist resorts including
Java.
- Malaysia
- Most areas including Kuala Lumpur and Penang.
- North
Korea - A few southern areas have limited risk.
- Philippines
- Low risk in main cities, Cebu, Bohol & Catanduanes.
No risk in Manilla.
- South
Korea - Limited risk in the extreme northwest.
- Sarawak
- (Borneo) except deep forest areas.
- Thailand
- Bangkok and main tourist areas including Pattaya,
Phuket, Krabi, Hua Hin, Koh Samui, Kanchanaburi, Damnoen
Sadouak, Ayutthaya, Sukhothai, Khon Kaen & Chiang
Mai.
|
Avoid
mosquito bites |
|
| Risk
variable. Some chloroquine resistance. |
- Indonesia
- Areas other than Bali and low risk cities, or Irian
Jaya and Lombok where the risk is high and chloroquine
resistance is present.
- Philippines
- Rural areas below 600 metres.
- Malaysia
and Sarawak (Borneo) - Deep forest regions of penninsular
Malaysia and Sarawak.
|
Chloroquine
PLUS
Proguanil |
Will
vary locally. |
Risk
substantial.
Chloroquine resistance common. |
- Borneo
- Sabah
- Cambodia
- Most of the country except Phnom Penh where there
is no risk.
- China
- Yunnan and Hainan provences only. All other remote
areas use chloroquine.
- East
Timor
- Irian
Jaya & Lombok
- Laos
- except Vientiane where there is no risk.
- Myanmar
- (formerly Burma).
- Sabah
- Part of Malaysia (Borneo)
- Vietnam
- Most rural areas, no risk in cities, Red River delta
area and the coastal plain north of Nha Trang.
|
Doxycycline
OR
Mefloquine
OR
Malarone
|
Chloroquine
PLUS
Proguanil |
|
Risk
great.
Chloroquine resistance prevalent. Some
mefloquine resistance reported
|
- Cambodia
- Western provences.
- Thailand
- Near borders with Cambodia & Myanmar. Koh Chang.
- Myanmar
- Eastern part of Shan state.
|
Doxycycline
OR
Malarone |
|
| Malaria
prophylaxis for Oceania |
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
Risk
high.
Chloroquine resistance high. |
- Papua
New Guinea - below 1,800 metres.
- Solomon
Islands
- Vanuatu
|
Doxycycline
OR
Mefloquine
OR
Malarone
|
Maloprim
PLUS
Chloroquine |
| Malaria
prophylaxis for South & Central America & the
Caribbean |
|
Risk
|
Country
|
Preferable
regimen
|
Alternative
regimen
|
| Risk
very low |
- Brazil
- Except the Amazon basin region, Mato Grosso &
Maranhao.
|
Avoid
mosquito bites. |
|
| Risk
variable to low, no chloroquine resistance present. |
- Argentina
- Rural areas along northern borders only.
- Belize
- Rural areas except Belize district.
- Costa
Rica - Rural areas below 500m.
- Dominican
Republic
- El
Salvador - Only Santa Ana province in the West.
- Guatamala
- Areas below 1,500 metres.
- Haiti
- The whole country.
- Honduras
- The whole country.
- Mexico
- Some rural areas rarely stayed in by tourists.
- Nicaragua
- The whole country.
- Panama
- West of the canal.
- Paraguay
- Some rural areas.
|
Chloroquine |
Proguanil |
| Risk
variable or high, some chloroquine resistance present.
|
- Bolivia
- Rural areas below 2,500 metres
- Ecuador
- Areas below 1,500 metres. No malaria in Galapagos
Islands nor in Guayaquil.
- Panama
- East of the canal.
- Peru
- Rural areas below 1,500 metres.
- Venezuela
- Rural areas other than the coast. Caracas is free
of malaria.
|
Proguanil
PLUS
Chloroquine |
Doxycycline
OR
Mefloquine
OR
Malarone |
Risk
high,
marked chloroquine resistance. |
- Brazil
- Amazon basin region, Mato Grosso & Maranhao
only. Very low risk and no chemoprophylazis required
elsewhere.
- Colombia
- Most areas below 800m
- Ecuador
- Esmeraldas Province.
- French
Guiana - Especially border areas.
- Guyana
- All interior regions.
- Surinam
- Except Paramaribo and coast.
- Amazon
basin areas of Bolivia, Venezuela and Peru.
|
Doxycycline
OR
Mefloquine
OR
Malarone
|
Proguanil
PLUS
Chloroquine |
 Treatment
of Malaria with Artemisinin Treatment
of Malaria with Artemisinin
Artemisinin is a powerful antimalarial compound
derived from the sweet wormwood plant (Artemisia Annua) and
has transformed the tratment of malaria
It is a natural plant compound. first isolated in 1972 by
Chinese scientist Professor Youyou Tu and her team from the
Artemisia Annua plant known as 'Qinghao' which has been used
in Chinese herbal medicine for over two millennia to treat
fever.
The sweet wormwood plant, originally
from Asia's temperate regions, particularly China is now grown
worldwide for its medicinal uses.
-
Artemisinin
helps significantly reduce the parasites but doesn't stay
in the body for a long time, being eliminated within hours.
It is usually partnered with another drug that eliminates
the remaining parasites over a longer period of time,
reducing treatment for P. falciparum malaria to 3 days.
-
Artesunate,
an artemisinin derivative, is highly effective at treating
severe malaria as it is the only artemisinin derivative
that can be given via intravenous injection. This allows
it to take immediate effect, clearing parasites rapidly,
an important priority in severely ill patients whose symptoms
can continue to deteriorate quickly.
-
Like
all antimalarials before it, resistance to artemisinin
will continue to grow, as parasites evolve. Strategies
for a better usage of existing ACTs and research into
non-artemisinin treatments are crucial to ensure we can
continue to treat this deadly disease into the future.
 Artemisinin
works mainly on the asexual blood stage, and particularly
the young-ring stage, a critical phase in the malaria parasite’s
lifecycle. Artemisinin
works mainly on the asexual blood stage, and particularly
the young-ring stage, a critical phase in the malaria parasite’s
lifecycle.
During this stage, parasites multiply quickly in the bloodstream
by consuming haemoglobin to get proteins for growth therby
increasing their numbers in the blood and causing the symptoms
of malaria.
When artemisinin is given, heme from broken-down hemoglobin
in the blood breaks artemisinin's endoperoxide bond. This
creates highly reactive oxygen particles that attack the malaria
parasites killing them.
The endoperoxide bond (a special chemical structure with a
peroxide group) is crucial for artemisinin's antimalarial
effects. However, we still don't fully understand how it works.
To boost its effectiveness, scientists have developed several
artemisinin derivatives, including dihydroartemisinin, artesunate,
and artemether.
Note:
Artemisinin is currently used to treat malaria rather
than as a prophylactic.
|