|
 Typhoid
Fever Typhoid
Fever
Typhoid fever is a life-threatening illness caused by the
bacterium Salmonella Typhi. It belongs to the Salmonella
group which contains nearly 2,000 different types causing
mild diseases such as food poisoning, through to the more
serious disease of typhoid fever. Paratyphoid fever
is a similar but less severe variant.
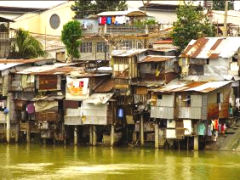
It is a common illness in the developing world, where it affects
about 12.5 million people each year.
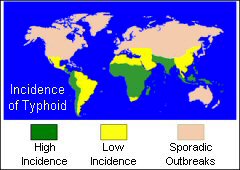
Typhoid fever occurs in most parts of the world except in
developed countries such as the United Kingdom, Western Europe,
USA, Canada, Australia, New Zealand and Japan. Therefore,
if you are traveling to the developing world, you should consider
taking precautions. Travellers to Asia, Africa, and Latin
America are especially at risk.
 The
typhoid fever bacteria is carried in the bloodstream and intestinal
tract of infected persons. A small number of persons, called
carriers, recover from the fever but continue to carry the
bacteria. Both ill persons and carriers shed the bacteria
in their feces. Diagnosis requires medical opinion and examination
of the blood. The
typhoid fever bacteria is carried in the bloodstream and intestinal
tract of infected persons. A small number of persons, called
carriers, recover from the fever but continue to carry the
bacteria. Both ill persons and carriers shed the bacteria
in their feces. Diagnosis requires medical opinion and examination
of the blood.
You can get typhoid fever if you eat food or drink beverages
that have been contaminated by a person who is shedding S.
Typhi or if sewage contaminated with S. Typhi bacteria
gets into the water you use for drinking or washing food.
Therefore, typhoid fever is more common in areas of the world
where handwashing is less frequent and water is likely to
be contaminated with sewage.
The incubation period depends on the quantity of the bacteria
swallowed and can vary from one to three weeks.
Persons with typhoid fever usually have a sustained fever
as high as 39° or 40° C. They will also feel weak, have stomach
pains, headache and loss of appetite. In some cases, patients
have a rash of flat, rose-colored spots.
 Treatment:
Typhoid fever is usually treated with antibiotics such as
ampicillin or ciprofloxacin which are very effective but should
ideally be given under medical supervision. Hospital admission
may be more appropriate abroad. Persons treated with antibiotics
usually improve within 2 to 3 days, and deaths rarely occur.
However, relapse is not uncommon and patients may develop
the carrier state after treatment. It is therefore very important
to have your stools examined on your return if you have been
treated for typhoid abroad. Treatment:
Typhoid fever is usually treated with antibiotics such as
ampicillin or ciprofloxacin which are very effective but should
ideally be given under medical supervision. Hospital admission
may be more appropriate abroad. Persons treated with antibiotics
usually improve within 2 to 3 days, and deaths rarely occur.
However, relapse is not uncommon and patients may develop
the carrier state after treatment. It is therefore very important
to have your stools examined on your return if you have been
treated for typhoid abroad.
Without treatment this illness can
be fatal!!. Persons who do not receive treatment
may continue to have the fever for weeks or months, and as
many as 20% may die from complications such as peritonitis
resulting from perforation of the gut wall.
 Typhoid
fever can be prevented and can usually be treated with antibiotics.
If you are planning to travel to a region where it exists,
you should know about it and what steps you can take to protect
yourself. Typhoid
fever can be prevented and can usually be treated with antibiotics.
If you are planning to travel to a region where it exists,
you should know about it and what steps you can take to protect
yourself.
There are two basic actions that can help to protect you from
typhoid fever:
1. Get vaccinated against typhoid fever.
2. Avoid risky foods and drinks.
Watching what you eat and drink when you travel is just as
important as being vaccinated. This is because the vaccines
are not completely effective. Avoiding risky foods will also
help protect you from other illnesses, including travelers'
diarrhoea, cholera, dysentery, and hepatitis A.
 Tetanus Tetanus
Tetanus is a potentially fatal disease which is caused by
an infection of the bacterium Clostridium Tetani. The
bacteria enter the body through a wound where they grow and
produce a powerful toxin which circulates in the blood and
causes muscular rigidity and painful muscle contractions.
Death is usually caused by respiratory problems and exhaustion.
 Tetanus
spores are present in soil worldwide and may be introduced
into the body during injury through a puncture wound, burn
or trivial, unnoticed wounds. Tetanus
spores are present in soil worldwide and may be introduced
into the body during injury through a puncture wound, burn
or trivial, unnoticed wounds.
Tetanus can be contracted quite easily through a small wound
such as a scratch through which the organism can get into
the body. There have been reported cases of tetanus in which
the patient cannot even remember the injury since it was so
small and insignificant.
 While
vaccination has largely diminished the incidence of tetanus,
the disease has not disappeared. While
vaccination has largely diminished the incidence of tetanus,
the disease has not disappeared.
If individuals are not fully immunised there is always the
risk of tetanus developing in wounds contaminated by soil.
The incubation period is between four and twenty one days,
commonly around ten days.
The first sign of tetanus is when the patient may notice jaw
stiffness and difficulty in opening the mouth (lock jaw).
Treatment: Requires medical supervision in hospital.
Prevention: All wounds, even minor ones should be thoroughly
washed with clean water and soap taking particular care to
remove all dirt and loose tissue.
 Immunisation
against tetanus is highly protective and adults and children
should ensure they are in date for it. Booster doses should
be given at ten year intervals. Immunisation
against tetanus is highly protective and adults and children
should ensure they are in date for it. Booster doses should
be given at ten year intervals.
Booster doses in addition to five doses are not recommended
except in the case of the treatment of a tetanus-prone wound.
The Department of Health advised in 2002 that tetanus vaccine
is to be replaced by the combined tetanus/low dose diphtheria
vaccine for adults and adolescents for routine use and for
travel vaccination. Stocks of single tetanus vaccine are now
exhausted and companies are no longer supplying this product.
 Poliomyelitis
(polio) Poliomyelitis
(polio)
Poliomyelitis, normally referred to as polio is caused by
a virus which is spread from person-to-person primarily through
faecal contamination of food and water although it can also
be spread by droplet transfer.
Initially, infection of the gut can spread to the spinal cord
or brain where it can cause paralysis. In the days before
widespread vaccination it tended to occur in epidemics.
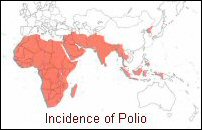 Travellers
who have not been immunised or whose immunity has waned are
at risk if they are travelling to areas of the world where
polio still occurs. ie. Nigeria, Niger, India, Pakistan and
Afghanistan are particularly high risk. Travellers
who have not been immunised or whose immunity has waned are
at risk if they are travelling to areas of the world where
polio still occurs. ie. Nigeria, Niger, India, Pakistan and
Afghanistan are particularly high risk.
In many cases infection with the polio virus is asymptomatic.
When symptoms do occur, the onset of polio is sudden with
fever, headache, nausea and vomiting as the virus multiplies
in the gut. The virus then invades the blood stream and nervous
system.
Paralysis occurs in less than 1 in 100 cases of infection.
This risk increases with age. The patient may die if the respiratory
and swallowing muscles are affected. Those who survive may
develop residual paralysis. Severe pain, and wasting are common
in paralysed muscles. Recovery can take up to a year.

The incubation period is 7-14 days. A blood test for antibodies
will confirm the diagnosis, although this is not always available
abroad. Patients are infectious by close contact and should
be isolated for at least a week.
Treatment: The development of paralysis is clearly
an emergency and medical help should be sought without delay.
If the paralysis affects the breathing muscles, artificial
means of respiration may be required. Extreme care should
be taken when disposing of excreta for up to 6 weeks.
Prevention: There is an effective vaccine available.
Ten yearly boosters should be given to ensure maximum immunity
and travellers should ensure they are in date for polio immunisation.
 Past
infection with polio does not always give complete protection
as there are three strains of the virus. Past
infection with polio does not always give complete protection
as there are three strains of the virus.
As the disease is usually spread through close contact, try
to avoid crowded places in high risk areas as much as possible.
(buses, trains,public swimming pools). This could prove difficult
in some countries such as India. Therefore vaccination would
be imperative if travelling there.
The World Health Organisation is making great efforts to encourage
widespread use of polio vaccine in an attempt to eradicate
polio from all the countries of the world. Many countries
have already been certified polio free by the WHO. By 1994,
the Americas were certified as polio-free.
 Hepatitis
A Hepatitis
A
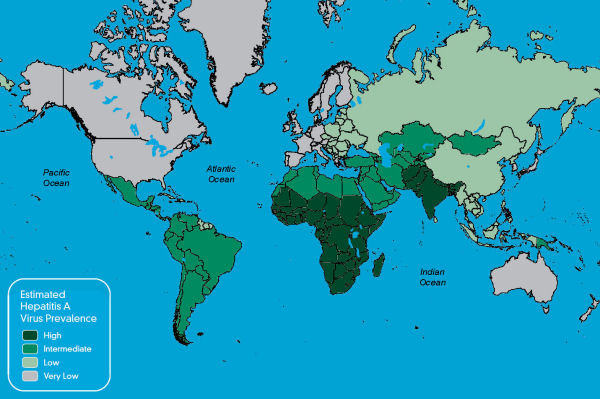
This is a viral disease that causes inflammation of the liver.
It occurs worldwide and is especially prevalent in areas of
poor sanitation and hygiene.
Many children in developing countries are infected with the
virus at an early age, usually without symptoms. Past infection
with hepatitis A virus gives life long immunity.
However, in the developed world where sanitation is better,
fewer people are contracting the disease during childhood
and are therefore at risk when they become adults from the
more severe form of the disease, which they could catch when
they travel to areas of the world where hepatitis A is more
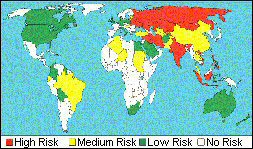
common. The map below shows the global incidence of Hepatitis
A.
The virus
is transmitted from person-to-person by the faecal-oral route
particularly in areas with poor sanitation and overcrowding.
It is quickly spread through close contact, particularly within
families and institutions and is commonly associated with
eating and drinking contaminated food and water. Food outbreaks
are often linked to raw or undercooked shellfish and raw vegetables
although almost any food can be implicated which has been
poorly cooked in sewage-polluted water.
 Hepatitis
A has a wide range of symptoms, from an infection without
any noticeable symptoms through to jaundice, liver failure
and death. Unlike hepatitis B, there is no chronic carrier
state for hepatitis A. Hepatitis
A has a wide range of symptoms, from an infection without
any noticeable symptoms through to jaundice, liver failure
and death. Unlike hepatitis B, there is no chronic carrier
state for hepatitis A.
Symptoms include fever, chills, weakness, loss of appetite,
nausea and abdominal discomfort, followed within a few days
by jaundice (yellowing of the skin and eyes). The urine becomes
dark and the stools pale. Jaundice may be severe and prolonged
and complete liver failure may occur.
Prevention: Avoid contaminated food and water.
Hepatitis A can be prevented by vaccination. The immunisation
schedule consists of a single dose of vaccine followed by
a booster dose six to twelve months after the first dose to
give immunity up to ten years.
 Cholera Cholera
Cholera is a bacterial infection of the gastro-intestinal
tract caused by the bacterium Vibrio Cholerae.
These bacteria are typically ingested by drinking water
contaminated by improper sanitation or by eating improperly
cooked fish, especially shell fish.
About one million Vibrio cholerae bacteria must be ingested
to cause cholera in normally healthy adults, although increased
susceptibility may be observed in those with weakened immune
systems, individuals with decreased gastric acidity (as from
the use of antacids etc.), or those who are malnourished.
The incubation period is usually two to three days but may
only be a few hours.
Symptoms range from the mild to the severe which may be
fatal and include; diarrhoea, abdominal cramps, nausea,
vomiting, and dehydration.
 Vibrio
cholerae causes the disease by producing a toxin that induces
severe painless watery diarrhoea of sudden onset, occasionally
accompanied by vomiting, which rapidly leads to dehydration.
The profuse diarrhoea allows the bacterium to spread
to other people under insanitary conditions. Vibrio
cholerae causes the disease by producing a toxin that induces
severe painless watery diarrhoea of sudden onset, occasionally
accompanied by vomiting, which rapidly leads to dehydration.
The profuse diarrhoea allows the bacterium to spread
to other people under insanitary conditions.
The bacteria are transmitted in water or food contaminated
with infected faeces and the disease can occur in large-scale
epidemics where sanitary conditions have broken down such
as those in areas of natural disasters.
Cholera is rare amongst travellers as they tend to avoid the
insanitary conditions which would put them at risk.
Treatment: Medical help should be sought without delay.
Cholera is treated with rehydration and antibiotics, but in
severe cases, can lead to death.
Fluid replacement is essential and should be started as soon
as symptoms occur. The patient should aim to drink as much
non-alcoholic fluid as it takes to maintain a good output
of normal looking urine (this may be as much as six or seven
litres a day).
Prevention: Avoid contaminated food and water, especially
raw or undercooked seafood from polluted water.
There is a new vaccine (Dukoral) for immunisation against
cholera for people travelling to highly endemic or epidemic
areas, particularly emergency relief and health workers in
refugee situations. The vaccine may be considered for the
following:
- People
working in areas where there are known cholera outbreaks
(e.g. aid workers).
- Travellers
staying for long periods in known high risk areas and/or
where close contact with locals is likely, and who do
not have access to medical care.
- Travellers
to risk areas who have an underlying gastro-intestinal
disease or immune suppression.
The vaccine
is taken as a raspberry flavoured drink and can be used in
adults and children over 2 years.
It is not currently licensed in the UK for travellers diarrhoea.
 Meningitis
(Meningococcal) Meningitis
(Meningococcal)
Meningitis
is an infection that causes inflamation of the membranes and
fluid that surrounds the brain and spinal cord. It can be
caused by a viral or bacterial infection.
Viral meningitis is generally less severe and resolves without
specific treatment, while bacterial meningitis (meningococcal)
can be quite severe and may result in brain damage, coma or
even death.
 It
can occur in epidemics, especially where large crowds are
gathered, as it is acquired through direct contact or inhalation
of bacteria in droplets coughed or sneezed into the air. It
can occur in epidemics, especially where large crowds are
gathered, as it is acquired through direct contact or inhalation
of bacteria in droplets coughed or sneezed into the air.
Early diagnosis and treatment are very important. If symptoms
occur, the patient should seek medical help immediately. Medical
supervision is required since large doses of antibiotics are
employed. Treatment should be started without delay. Identification
of the type of bacteria responsible is helpful for the selection
of correct antibiotics.
High fever, headache, and stiff neck and a blotchy rash are
common symptoms. These can develop over several hours, or
they may take 1 to 2 days. Other symptoms may include nausea,
vomiting, discomfort with bright lights, confusion, and sleepiness.
As the disease progresses, patients may develop seizures before
going into a coma.
 Sporadic
cases of meningitis are found worldwide. In temperate zones,
most cases occur in the winter months. Localized outbreaks
occur in enclosed crowded spaces (e.g. dormitories, military
barracks). In sub-Saharan Africa, in a zone stretching across
the continent from Senegal to Ethiopia (known as the African
“meningitis belt”), large outbreaks and epidemics take place
during the dry season (November–June). Sporadic
cases of meningitis are found worldwide. In temperate zones,
most cases occur in the winter months. Localized outbreaks
occur in enclosed crowded spaces (e.g. dormitories, military
barracks). In sub-Saharan Africa, in a zone stretching across
the continent from Senegal to Ethiopia (known as the African
“meningitis belt”), large outbreaks and epidemics take place
during the dry season (November–June).
Bacterial
meningitis is contagious. The bacteria are spread by direct
person to person contact including aerosol transmission and
exchange of respiratory and throat secretions (i.e. sneezing,
coughing, kissing, etc.).
Fortunately, none of the bacteria that cause meningitis are
as contagious as the viruses that spread the common cold or
influenza, and they are not spread by casual contact or by
simply breathing the air where a person with meningitis has
been.
 The
risk to travellers is generally low. However, the risk is
considerable if travellers are in crowded conditions or taking
part in large population movements such as pilgrimages eg.
the Haj to Mecca. Localized outbreaks occasionally occur among
travellers (usually young adults) in camps or dormitories.
Backpackers who use crowded hostels will be at greater risk
during an outbreak The
risk to travellers is generally low. However, the risk is
considerable if travellers are in crowded conditions or taking
part in large population movements such as pilgrimages eg.
the Haj to Mecca. Localized outbreaks occasionally occur among
travellers (usually young adults) in camps or dormitories.
Backpackers who use crowded hostels will be at greater risk
during an outbreak
Prevention:
Avoid overcrowded places and close contact with the local
population.
There are two vaccines used to protect travellers. The meningitis
A + C vaccine and the meningitis ACWY vaccine. The latter
is required for pilgrims and seasonal workers visiting Saudi
Arabia.
Effective treatment is undertaken with a number of antibiotics.
It is important, however, that treatment be started early
in the course of the disease. This will reduce the risk of
mortality to below 15%, although the risk is higher among
the elderly.
 Diphtheria Diphtheria
Diphtheria is an infection caused by a bacterium called Corynebacterium
diphtheriae that causes a moderately sore throat. Sometimes
the lining of the throat may swell to form "a false membrane"
which can cause difficulties in breathing.
In its early stages, diphtheria may be mistaken for a severe
sore throat. In severe cases the neck tissue may become very
swollen and in tropical countries the infection can occur
in skin ulcers.
It is mainly spread by droplets expelled from the nose and
mouth usually by breathing in diphtheria bacteria after an
infected person has coughed, sneezed or even laughed. It can
also be spread by handling used tissues or by drinking from
a glass used by an infected person.
 Nearly
one out of every ten people who get diphtheria will die from
it. Most cases occur among unvaccinated or inadequately vaccinated
people. Nearly
one out of every ten people who get diphtheria will die from
it. Most cases occur among unvaccinated or inadequately vaccinated
people.
The bacterium produces a toxin which can seriously damage
the heart muscle and the nervous system.
After two to six weeks, the effects of the toxin produced
by the bacteria become apparent with severe muscle weakness,
mainly affecting the muscles of the head and neck. Inflammation
of the heart muscle can cause heart failure.
Death usually occurs either from respiratory failure, heart
failure or a build up of toxin in the nervous system.
 Whether
or not the patient dies depends on the severity of the illness,
their level of immunity and the speed with which treatment
is started. Whether
or not the patient dies depends on the severity of the illness,
their level of immunity and the speed with which treatment
is started.
One of the regions where diphtheria is present is eastern
Europe, including Russia and the former states of the Soviet
Union. Cases of have occurred in Finland, Estonia, Poland
and Belarus and even Germany, Belgium and the UK resulting
from imported infection.
Treatment: This is specialised and requires medical
supervision in hospital.
 Prevention:
Try to avoid too close contact with people in crowded
places when travelling in endemic regions (particularly kissing
and sharing bottles or glasses). Prevention:
Try to avoid too close contact with people in crowded
places when travelling in endemic regions (particularly kissing
and sharing bottles or glasses).
Diphtheria can be prevented with a safe and effective vaccine.
A vaccine is now available for travellers to provide protection
against both diphtheria and tetanus.
Immunisation is very effective and UK children are immunised
within their first year. Boosters are required every 10 years
for travellers and those at risk.
 Rabies Rabies
This is a viral infection that is acquired from the saliva
of an infected or rabid animal, usually a dog or cat. In most
cases infection results from a bite but even a lick on an
open cut or sore may be enough.
Symptoms start with itching and tingling at the site of the
healed bite and then rapidly progresses to include headache,
fever, spreading paralysis, confusion, aggression and hydrophobia
(fear of water).
It may take many weeks or months for symptoms to develop although
it is usually two to eight weeks. Animals may be infectious
for five days before they develop symptoms.
Treatment: Thoroughly cleanse all bites with soap and
water and do not allow the wound to be stitched. Limited bleeding
should be encouraged. Apply alcohol if possible.
 If
available human immunoglobulin (HRIG) should be given especially
for bites to the head/face. The disease can almost always
be prevented, even after exposure, if the vaccine is administered
without delay. If
available human immunoglobulin (HRIG) should be given especially
for bites to the head/face. The disease can almost always
be prevented, even after exposure, if the vaccine is administered
without delay.
You should therefore seek medical advice immediately and have
a course of 5 injections of Purified Chick Embryo Cell Vaccine
(PCEC) or Human Diploid Cell Vaccine (HDCV). This can be difficult
to obtain abroad and if necessary the British Embassy or consulate
should be contacted for a supply.
If you have had a pre-exposure course of vaccine you should
still have a 'booster' course of 2 doses of vaccine without
delay.
Prevention: Never approach or handle animals you don't
know, particularly if they are acting strangely.
Pre-exposure immunisation against rabies is recommended for
long-stay travellers/residents and those who intend to travel
to rural and remote areas.
In the event of a bite, your body's responses could be quickly
activated by booster doses of vaccine. There are rarely any
side effects or discomfort from the new type of vaccine unlike
the old types.
 Tuberculosis
(TB) Tuberculosis
(TB)
Tuberculosis
(TB) is an airborne, infectious disease caused by a bacterium
called Mycobacterium tuberculosis which primarily affects
the lungs.
While both preventable and curable, TB remains one of the
world’s major causes of illness and death.
Approximately one-third of the world’s population carry
the TB bacteria, almost 9 million of whom develop “active”
TB each year, which can then be spread to others.
The disease is usually spread through infected sputum but
there is a form spread through milk from infected cows.
 Transmission
is usually spread by inhalatation of microscopic droplets
that come from a person infected with TB. When coughing, speaking
or sneezing, small droplets are expelled into the air which
quickly dry out but the bacteria can remain airborne for hours. Transmission
is usually spread by inhalatation of microscopic droplets
that come from a person infected with TB. When coughing, speaking
or sneezing, small droplets are expelled into the air which
quickly dry out but the bacteria can remain airborne for hours.
After the tuberculosis bacteria have been inhaled, they invade
the lungs, and within approximately six weeks a small infection
appears which rarely gives any symptoms but sometimes general
malaise, weakness and weight loss are characteristic during
the incubation period which may be up to twelve weeks. After
this, the bacteria can then spread through the blood.
The infection remains dormant in most cases in people who
are otherwise healthy and does not do any obvious harm. Months
or even years later, however, the disease can become reactivated
in different organs if the immune system is weakened. The
lungs are the favourite place for the illness to strike.
Typical symptoms of TB include:
- Having
a persistent cough for more than three weeks that brings
up phlegm, which may be bloody.
- High
temperature (fever).
- Weight
loss.
- Loss
of appetite
- Night
sweats.
- Tiredness
and fatigue.
TB usually
develops slowly and symptoms might not begin until months
or even years after initial exposure to the bacteria.
 In
some cases the bacteria infect the body but don't cause any
symptoms, which is known as latent TB. If the bacteria do
cause symptoms it is active TB. In
some cases the bacteria infect the body but don't cause any
symptoms, which is known as latent TB. If the bacteria do
cause symptoms it is active TB.
You should see a GP if you have a cough that lasts more than
three weeks or if you cough up blood or have any of the above
symptoms and have been in contact with someone who has the
disease.
The
bacteria can spread to the blood in individuals who have weak
immune systems (especially when caused by alcohol or HIV).
TB is primarily a disease of the lungs. However, the infection
can spread via blood from the lungs to other organs in the
body, the bones, the urinary tract and sexual organs, the
intestines and even in the skin. Lymph nodes in the lungs
and throat can also get infected.
 Sometimes
the disease can be overwhelming; producing meningitis and
coma; this particularly dangerous form is usually found in
children and those who have not previously been vaccinated
or exposed to the disease. Sometimes
the disease can be overwhelming; producing meningitis and
coma; this particularly dangerous form is usually found in
children and those who have not previously been vaccinated
or exposed to the disease.
TB is found in every country in the world, but the majority
of TB cases are concentrated in developing countries, particularly
those in Asia and Africa. It is a serious condition but can
be cured with proper treatment.
Three million deaths occur each year from TB, which is more
than any other single infectious disease. The disease is more
common in areas of the world where poverty, malnutrition,
poor general health and social disruption are present. The
disease has been commonly found in places of crowding such
as hostels and prisons where healthcare is poor.
 Treatment:
Treatment with antibiotics is effective but is prolonged. Treatment:
Treatment with antibiotics is effective but is prolonged.
Effective and affordable antimicrobial drugs to treat TB disease
have been available for decades but these must be taken for
six to eight months under medical supervision because if treatment
is not completed, the emergence of drug-resistant strains
of the TB bacteria may be encouraged. These medicines may
not always available abroad.
With treatment, a TB infection can usually be cured. Several
different antibiotics are used. This is because some forms
of TB are resistant to certain antibiotics. If you are infected
with a drug-resistant form of TB, treatment can last as long
as 18 months.
The usual course of treatment is:
- Two
antibiotics – isoniazid and rifampicin – every
day for six months.
- Two
additional antibiotics – pyrazinamide and ethambutol
– every day for the first two months.
 After
taking the medicine for two weeks, most people are no longer
infectious and feel much better. However, it is important
to continue taking the medicine exactly as prescribed and
to complete the whole course of antibiotics. After
taking the medicine for two weeks, most people are no longer
infectious and feel much better. However, it is important
to continue taking the medicine exactly as prescribed and
to complete the whole course of antibiotics.
It may be several weeks or months before a person starts to
feel better. The exact length of time will depend on your
overall health and the severity of your TB.
If you have been in close contact with someone who has TB,
tests may be carried out to see if you are also infected.
These can include a chest X-ray, sputum tests, blood tests
and a skin test.
Prevention:
Travelers should try to avoid exposure to TB patients in crowded
environments (such as hospitals, prisons, or homeless shelters).
Avoid other overcrowded places, particularly where spitting
is common.
The risk of TB transmission on an aeroplane does not appear
to be higher than in any other enclosed space.
To prevent TB transmission, people who have infectious TB
should not travel by commercial aircraft or other commercial
conveyances.
Never drink unpasteurised milk. If in doubt, boil it before
drinking.
There is a vaccination against TB which can give a valuable
degree of protection, particularly in children.
Those who have not received BCG immunisation are advised to
do so and if for travel purposes, at least six weeks before
departure to ensure a protective level of immunity.
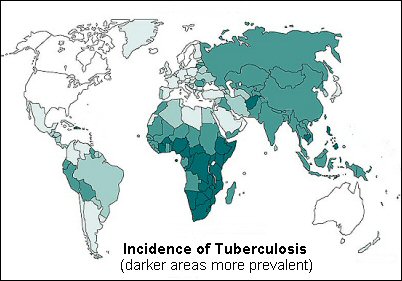
Click on this map to see a larger
map
 Schistosomiasis Schistosomiasis
Also
known as bilharzia, is a disease caused by parasitic worms
called schistosoma. They belong to the family of flat worms
known as trematodes or flukes. There are several different
species e.g. S. mansoni, S. haematobium, and S. japonicum.
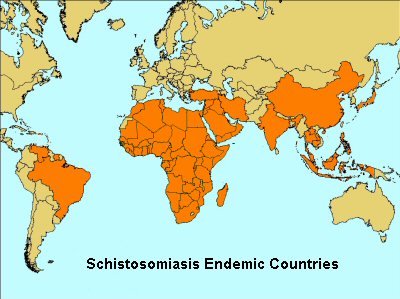
About 200 million people are thought to be infected world-wide.
The infection occurs when the skin comes into contact with
contaminated fresh water which contains a certain type of
snail that carry the schistosomes.
Fresh water becomes contaminated by Schistosoma eggs when
people who are infected urinate or defaecate in the water.
The eggs then hatch, and if the snails are present in the
water, the parasites invade the snails and grow and develop
inside them. The parasites eventually leaves the snails and
enter the water where they can survive for up to 48 hours.
 Schistosoma
parasites can penetrate the skin of persons who are wading,
swimming, bathing, or washing in contaminated water. Within
several weeks, worms grow inside the blood vessels of the
body and produce eggs. Some of these eggs travel to the bladder
or intestines and are passed into the urine or stools. Schistosoma
parasites can penetrate the skin of persons who are wading,
swimming, bathing, or washing in contaminated water. Within
several weeks, worms grow inside the blood vessels of the
body and produce eggs. Some of these eggs travel to the bladder
or intestines and are passed into the urine or stools.
Symptoms:
Within days after becoming infected, a rash or itchy skin
may develop. Fever, chills, cough, and muscle aches can begin
within 1-2 months of infection. Most people have no symptoms
at this early phase of infection.
Eggs travel to the liver or pass into the intestine or bladder.
Rarely, eggs are found in the brain or spinal cord and can
cause seizures, paralysis, or spinal cord inflammation. For
people who are repeatedly infected for many years, the parasite
can damage the liver, intestines, lungs, and bladder.
The symptoms of schistosomiasis are caused by the body's reaction
to the eggs, not by the worms themselves.
 Anyone
travelling to areas where schistosomiasis occurs and whose
skin comes in contact with fresh water from canals, rivers,
streams, or lakes, is at risk of getting schistosomiasis. Anyone
travelling to areas where schistosomiasis occurs and whose
skin comes in contact with fresh water from canals, rivers,
streams, or lakes, is at risk of getting schistosomiasis.
If someone does develop any of the symptoms after visiting
one or more of the countries where schistosomiasis is found
and was in contact with fresh water, they should go immediately
to their doctor and describe in detail where and for how long
they travelled and that they may have been exposed to contaminated
water.
They will need to provide a stool or urine sample for analysis
to see if you the parasites are present. A blood test has
also been developed but there should be a six to eight week
interval after the last exposure to contaminated water before
the blood sample is taken.
Prevention:
 |
- Avoid
swimming or wading in fresh water when you are in
countries in which schistosomiasis occurs. Swimming
in the ocean and in chlorinated swimming pools is
generally thought to be safe.
-
Drink safe water. Because there is no way to make
sure that water coming directly from canals, lakes,
rivers, streams or springs is safe, you should either
boil water for 1 minute or filter the water before
drinking it.
- Boiling
water for at least 1 minute will kill any harmful
parasites, bacteria, or viruses present. Iodine
treatment alone WILL NOT GUARANTEE that water is
safe and free of all parasites
- Bath
water should be heated for 5 minutes at 65 degrees
Celsius. Water held in a storage tank for at least
48 hours should be safe for showering.
- Vigorous
towel drying after an accidental, very brief water
exposure may help to prevent the Schistosoma parasite
from penetrating the skin but you should NOT rely
on vigorous towel drying to prevent schistosomiasis.
- There
is no vaccine available.
|
|

|
 Treatment:
A safe and effective treatment of schistosomiasis is available.
Praziquantel is effective against all human schistozomes.
Treatment is usually for one or two days and no serious toxic
effects have been reported. Treatment:
A safe and effective treatment of schistosomiasis is available.
Praziquantel is effective against all human schistozomes.
Treatment is usually for one or two days and no serious toxic
effects have been reported.
Areas
of the world where schistosomiasis occurs:-
Africa: north Africa, southern Africa, sub-Saharan
Africa, Lake Malawi, the Nile River valley in Egypt.
South America: including Brazil, Surinam, Venezuela.
Caribbean: Antigua, Dominican Republic, Guadeloupe,
Martinique, Montserrat, Saint Lucia.
The Middle East: Iran, Iraq, Saudi Arabia, Syria &
Yemen.
Southeast Asia: India, Bagladesh, Central Indonesia,
the Philippines, Thailand, Laos, Cambodia, Vietnam (the Mekong
Delta), Southern China & Japan.
 Leptospirosis
(Weil's disease) Leptospirosis
(Weil's disease)
Leptospirosis is a bacterial disease
caused by bacteria of the genus Leptospira. It
affects humans and animals and causes
a wide range of symptoms, including high fever, severe headache,
chills, muscle aches, and vomiting, and may include, red eyes,
abdominal pain, diarrhea, or a rash although
some infected persons may have no symptoms at all. If
the disease is not treated, then kidney damage, meningitis
liver failure, respiratory distress and even death may result.
Outbreaks of leptospirosis are usually caused by exposure
to water contaminated with the urine of infected animals.
Many different kinds of animals carry the bacteria such as
cattle, pigs, horses, dogs, rodents, and wild animals.
 Humans
become infected through contact with water, food, or soil
containing urine from these infected animals. This may happen
by swallowing contaminated water or through cuts and contact
with broken skin. The disease is not spread from person to
person. Humans
become infected through contact with water, food, or soil
containing urine from these infected animals. This may happen
by swallowing contaminated water or through cuts and contact
with broken skin. The disease is not spread from person to
person.
The incubation period is anything from two days to four weeks.
The illness usually begins abruptly with fever and other symptoms.
Leptospirosis may occur in two phases; after the first phase,
with fever, chills, headache, muscle aches, vomiting, or diarrhoea,
the patient may recover for a time but become ill again.
If a second phase occurs, it is more severe; the person may
have kidney or liver failure or meningitis. This phase is
also called Weil's disease. Diagnosis of Leptospirosis is
confirmed by laboratory testing of a blood or urine sample.
 Leptospirosis
occurs worldwide but is most common in temperate or tropical
climates. It is an occupational hazard for many people who
work with animals, such as farmers, sewer workers, veterinarians,
fish workers, dairy farmers, or military personnel. Leptospirosis
occurs worldwide but is most common in temperate or tropical
climates. It is an occupational hazard for many people who
work with animals, such as farmers, sewer workers, veterinarians,
fish workers, dairy farmers, or military personnel.
It is a recreational hazard for campers or those who participate
in outdoor sports in contaminated areas and has been associated
with swimming, wading, and whitewater rafting in contaminated
lakes and rivers.
Leptospirosis can be effectively treated with antibiotics,
such as doxycycline or penicillin, which should be given as
early as possible in the course of the disease. Intravenous
antibiotics may be required for persons with more severe symptoms.
Persons who are thought to have symptoms suggestive of leptospirosis
should seek medical help immediately.
Ebola
Virus, Lassa Fever & Marburg Virus (the really nasty viruses)
Ebola
Virus
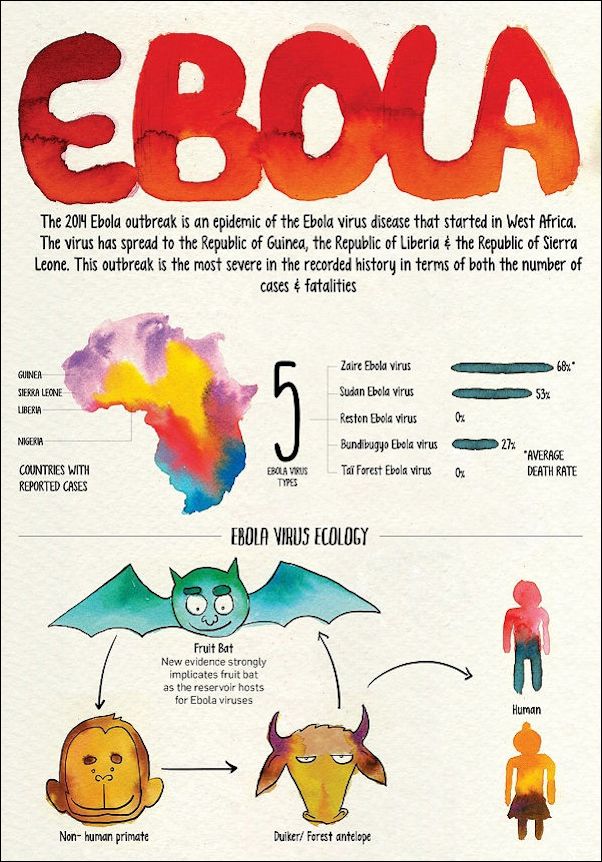
 Ebola
Hemorrhagic Fever is a severe, often-fatal disease that
has appeared sporadically since its initial recognition in
1976. Ebola
Hemorrhagic Fever is a severe, often-fatal disease that
has appeared sporadically since its initial recognition in
1976.
The disease is caused by infection with Ebola virus, named
after a river in the Democratic Republic of the Congo in West
Africa, where it was first recognized. The virus is one of
two members of a family of RNA viruses called the Filoviridae.
There are four identified subtypes of Ebola virus. Three of
which have caused disease in humans.
Infections with Ebola virus are acute. There is no carrier
state. Because the natural reservoir of the virus is unknown,
the manner in which the virus first appears in a human at
the start of an outbreak has not been determined. However,
it is thought that the first patient becomes infected through
contact with an infected animal, possibly a primate or a fruit
bat. Infection can occur from ingestion of infected meat.
Most of the previous outbreaks have been caused by meat from
dead infected animals collected by hunters who then sell it
on. Fruit
bats are also widely eaten in rural west Africa – either
smoked, grilled or in a spicy soup.
After
the first patient in an outbreak setting is infected, the
virus can be transmitted in several ways. People can be exposed
to Ebola virus from direct contact with the blood and/or secretions
of an infected person. Thus, the virus is often spread through
families and friends because they come in close contact with
such secretions when caring for infected persons. People can
also be exposed to Ebola virus through contact with objects,
such as needles, that have been contaminated with infected
secretions. Health workers who treat ebola patients are also
at risk and should always wear specialised protective clothing
when treating an infected person.
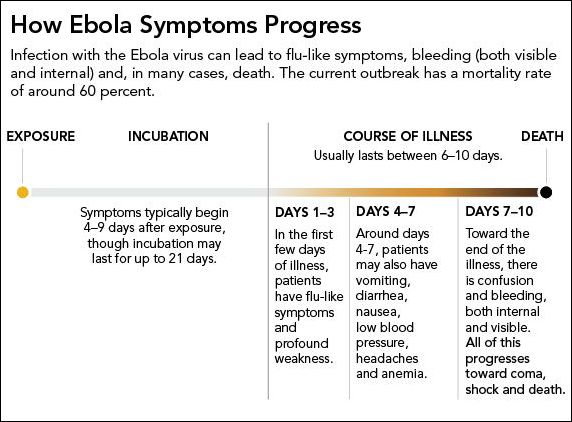
 The
incubation period for Ebola HF ranges from 2 to 21 days. The
onset of illness is abrupt and is characterized by fever,
headache, joint and muscle aches, sore throat, and weakness,
followed by diarrhoea, vomiting, and stomach pain. A rash,
decreased kidney and liver functioning, red eyes, hiccups
and internal and external bleeding may be seen in some patients. The
incubation period for Ebola HF ranges from 2 to 21 days. The
onset of illness is abrupt and is characterized by fever,
headache, joint and muscle aches, sore throat, and weakness,
followed by diarrhoea, vomiting, and stomach pain. A rash,
decreased kidney and liver functioning, red eyes, hiccups
and internal and external bleeding may be seen in some patients.
Researchers do not understand why some people are able to
recover from Ebola HF and others are not. However, it is known
that patients who die usually have not developed a significant
immune response to the virus at the time of death.
There is no standard treatment for Ebola HF. Patients must
be isolated and receive supportive therapy. This consists
of balancing the patient’s fluids and electrolytes, maintaining
their oxygen status and blood pressure, and treating them
for any complicating infections.
 How
Ebola kills: How
Ebola kills:
Once
the Ebola virus makes its way into the body, it gets into
the body's cells and replicates itself. Then it comes bursting
out of the cells and produces a protein called ebolavirus
glycoprotein that wreaks havoc. The ebolavirus glycoprotein,
attaches to the cells on the inside of blood vessels. This
increases the permeability of the blood vessels leading to
blood leaking out of the vessels. The virus also disrupts
the body's ability to coagulate and thicken the blood. Even
people who don't show hemorrhagic symptoms will experience
this leaking of blood from the vessels which can eventually
lead to shock and, ultimately, death.
 The
Ebola virus is also a master of evading the body's natural
defences: It blocks the signaling to cells called neutrophils,
which are white blood cells that are in charge of raising
the alarm for the immune system to come and attack. In fact,
Ebola will infect immune cells and travel in those cells to
other parts of the body, including the liver, kidney, spleen
and brain. The
Ebola virus is also a master of evading the body's natural
defences: It blocks the signaling to cells called neutrophils,
which are white blood cells that are in charge of raising
the alarm for the immune system to come and attack. In fact,
Ebola will infect immune cells and travel in those cells to
other parts of the body, including the liver, kidney, spleen
and brain.
Each time one of the cells is infected with the Ebola virus
and bursts open spilling out its contents, the damage and
presence of the virus particles activates molecules called
cytokines. In a healthy body, these cytokines are responsible
for provoking an inflammatory response so that the body knows
it's being attacked. But in the case of an Ebola patient it
is the overwhelming release of cytokines which cause the flu-like
symptoms that are the first sign of Ebola infection.
 The prevention
of Ebola HF in Africa presents many challenges. Because the
identity and location of the natural reservoir of Ebola virus
are unknown, there are few established primary prevention
measures.
The prevention
of Ebola HF in Africa presents many challenges. Because the
identity and location of the natural reservoir of Ebola virus
are unknown, there are few established primary prevention
measures.
There is currently no vaccine that protects against the
Ebola virus.
Education
regarding infection control measures to prevent the spread
of the virus is of paramount importance.
Unless you are travelling to an area where an Ebola outbreak
is occurring and/or you have direct contact with an ill individual
infected with Ebola, the risk of acquiring Ebola virus is
extremely low.
 Lassa
fever Lassa
fever
is an acute viral illness that occurs in West Africa.
The illness was discovered in 1969 and named after the town
in Nigeria where the first cases originated. The virus, a
member of the virus family Arenaviridae is animal-borne
and is acquired from a particular kind of wild rodent known
as the multimammate rat.
In the areas of Africa where the disease is endemic, Lassa
fever is a significant cause of mortality. While it is mild
or has no observable symptoms in about 80% of people infected,
the remaining 20% contract a severe multisystem disease. Lassa
fever is also associated with occasional epidemics, during
which the case-fatality rate can reach 50%.
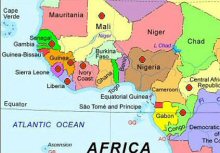 The
disease is known to be endemic (constantly present) in Nigeria,
Sierra Leone, Liberia, Guinea and the Central African Republic,
and there is evidence of infection in nearby countries including
Mali, Senegal, and the Democratic Republic of Congo. However,
because the rodent species which carry the virus are found
throughout West Africa, the actual geographic range of the
disease may extend to other countries in the region. The
disease is known to be endemic (constantly present) in Nigeria,
Sierra Leone, Liberia, Guinea and the Central African Republic,
and there is evidence of infection in nearby countries including
Mali, Senegal, and the Democratic Republic of Congo. However,
because the rodent species which carry the virus are found
throughout West Africa, the actual geographic range of the
disease may extend to other countries in the region.
The virus is shed in the urine and droppings of infected rats
(which are infected for life), and most infections arise through
contact with materials contaminated by these.
 Lassa
fever may also spread through person-to-person contact. This
type of transmission occurs when a person comes into contact
with virus in the blood, tissue, secretions, or excretions
of an individual infected with the Lassa virus. Lassa
fever may also spread through person-to-person contact. This
type of transmission occurs when a person comes into contact
with virus in the blood, tissue, secretions, or excretions
of an individual infected with the Lassa virus.
The virus cannot be spread through casual contact (including
skin-to-skin contact without exchange of body fluids). The
virus is present in semen for up to three months after the
disease begins, thus sexual transmission can also occur. It
may also be spread by contaminated medical equipment, such
as reused needles etc.
Marburg
Virus
 Marburg haemorrhagic fever is a rare, severe type of haemorrhagic
fever which affects both humans and animals. It is caused
by a genetically unique RNA virus of the filovirus family,
and its recognition led to the creation of this virus family.
The Ebola virus is the only other known member of this family.
Marburg haemorrhagic fever is a rare, severe type of haemorrhagic
fever which affects both humans and animals. It is caused
by a genetically unique RNA virus of the filovirus family,
and its recognition led to the creation of this virus family.
The Ebola virus is the only other known member of this family.
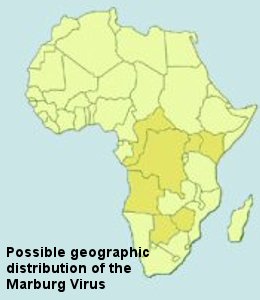
Marburg
virus is indigenous to Africa but the actual geographic area
to which it is native is unknown, but could include parts
of Uganda and Western Kenya, and Zimbabwe. As with Ebola virus,
the actual animal host for Marburg virus also remains a mystery.
Just
how the virus is first transmitted to humans is unknown. However,
as with some other viruses which cause haemorrhagic fever,
humans who become ill with Marburg fever may spread it to
other people.
After
an initial incubation period of five to ten days, the onset
of the disease is sudden and is marked by fever, chills, headache,
and myalgia. Around the fifth day after the onset of symptoms,
a rash appears, most prominent on the chest, back, stomach.
Nausea, vomiting, a sore throat, chest pain, abdominal pain,
and diarrhoea may then appear. Symptoms become increasingly
severe and may include jaundice, inflammation of the pancreas,
severe weight loss, delirium, shock, liver failure, multi-organ
dysfunction and even death.
Because
many of the signs and symptoms of Marburg fever are similar
to those of other diseases, such as malaria or typhoid fever,
diagnosis of the disease can be difficult, especially if only
a single case is involved.
 A
specific treatment for this disease is unknown. However, supportive
hospital therapy is required. This includes balancing the
patient's fluids and electrolytes, replacing lost blood and
clotting factors, maintaining their blood pressure, and treating
them for any complicating infections. A
specific treatment for this disease is unknown. However, supportive
hospital therapy is required. This includes balancing the
patient's fluids and electrolytes, replacing lost blood and
clotting factors, maintaining their blood pressure, and treating
them for any complicating infections.
Due to
our limited knowledge of the disease, preventive measures
against transmission from the original animal host have not
yet been established. Measures for prevention of secondary
transmission are similar to those used for other haemorrhagic
fevers.
People
who have close contact with infected humans or animals are
most at risk.
|