|
 When
entering a region where any of the
above diseases or indeed any disease spread by biting arthropods
is endemic, you should always take adequate precautions to
avoid being bitten or to reduce the number of bites. When
entering a region where any of the
above diseases or indeed any disease spread by biting arthropods
is endemic, you should always take adequate precautions to
avoid being bitten or to reduce the number of bites.
Besides the number of infections that can be caught from insect
bites, there is also the possibility of itchy weals caused
by reactions to the bites themselves.
Exposure to arthropod bites may be reduced if travellers follow
the advice below:
Repellents for use on clothing and skin:
Optimum protection can be provided by applying repellents
to clothing and to exposed skin. Products
containing the following active ingredients typically provide
reasonably long-lasting protection:
-
DEET:
Insect repellents made with a chemical called DEET (N,
N-diethyl-m-toluamide) work best. They are available as
creams, lotions and sprays and come in several strengths.
However, you don’t need to use anything stronger
than 50% DEET.
Research and experience have shown that DEET is very safe
when you follow the manufacturer’s instructions.
Up to 50% DEET can be used by pregnant or breast-feeding
women and for babies/children older than two months.
DEET is not usually recommended for babies under this
age. If you are taking a baby under two months to a country
with malaria and/or yellow fever, get expert advice about
suitable repellents.
The best advice is for pregnant women or young infants
to avoid such areas unless absolutely necessary.
-
Picaridin:
Alternative recommended insect repellents are those containing
Picaridin 20% and these can be used for children aged
two years and older.
-
Oil
of lemon eucalyptus -based repellent is also available
however this repellent only lasts as long as 15% DEET
and so needs applying more frequently. Note: Lemon eucalyptus
essential oil is a different product and is not recommended
as an insect repellent.
 Using
insect repellents: Using
insect repellents:
- Follow
the manufacturer’s instructions carefully.
- Apply
directly to any exposed areas of skin.
- Avoid
spraying directly onto your face to stop repellent getting
into your eyes, nose and mouth.
- Use
a cream/lotion or spray repellent on your hands and then
rub onto your face.
- Re-apply
regularly, especially after swimming and in hot, humid countries,
as sweating reduces effectiveness.
- Don’t
swallow repellent.
- Don’t
apply to cuts, grazes or broken/irritated skin.
- If
you are using sunscreen, put it on first.
- Sunscreen
containing repellent is not recommended.
- Wash
your hands after applying.
Clothing:
- Wear
loose fitting, light coloured clothes (insects can reach
skin through tight clothing), long trousers and long sleeves.
Don’t go barefoot.
- Malaria
mosquitoes are most active after dark, so it’s important
to cover up in the evenings in malaria risk regions.
- In
tick-infested areas, avoid shorts/skirts and tuck trousers
into socks and wear closed shoes instead of sandals to stop
ticks crawling up your legs or biting your feet.
- Many
insects can bite through thin clothing, so spray them with
an insecticide or repellent (such as permethrin - an insecticide
that kills insects on contact) but never use it directly
on your skin.
 Be
aware of peak exposure times and places: though mosquitoes
may bite at any time of day, peak biting activity for the
vectors of some diseases such as dengue and yellow fever is
during daylight hours whereas the vectors of other diseases
such as malaria are more active during twilight periods or
in the evening after dark (dawn and dusk). Be
aware of peak exposure times and places: though mosquitoes
may bite at any time of day, peak biting activity for the
vectors of some diseases such as dengue and yellow fever is
during daylight hours whereas the vectors of other diseases
such as malaria are more active during twilight periods or
in the evening after dark (dawn and dusk).
Focusing your preventive actions during peak hours may reduce
bite risk. Location also matters; ticks are often found in
grasses and other vegetated areas. Local guides may be able
to point out areas where there is increased arthropod activity.
Check for ticks: Travellers should inspect themselves
and their clothing for ticks during and following outdoor
activity. Prompt removal of attached ticks can prevent some
infections.
 Bed
nets (mosquito nets): When accommodations are not adequately
screened or air conditioned, bed nets are essential to provide
protection and to reduce discomfort caused by biting insects.
If bed nets do not reach the floor, they should be tucked
under mattresses. Bed nets are most effective when they are
treated with permethrin. Bed
nets (mosquito nets): When accommodations are not adequately
screened or air conditioned, bed nets are essential to provide
protection and to reduce discomfort caused by biting insects.
If bed nets do not reach the floor, they should be tucked
under mattresses. Bed nets are most effective when they are
treated with permethrin.
Pretreated nets can be purchased before travelling or nets
can be treated after purchase. Nets treated with a pyrethroid
insecticide will be effective for several months if they are
not washed. Long-lasting pretreated nets may be effective
for much longer.
Insecticides and spatial repellents: An increasing
array of products to be used as spatial repellents (containing
active ingredients such as metofluthrin and allethrin) are
becoming commercially available. These augment the aerosol
insecticides, vaporizing mats, and mosquito coils that have
been available for some time. Such products can help to clear
rooms or areas of mosquitoes (spray aerosols) or repel mosquitoes
from a circumscribed area (coils, spatial repellents).
However, travellers should supplement the use of these products
with topical or clothing repellents or bed nets in areas where
the potential for insect borne disease transmission is high
or if biting arthropods are noted.
Insecticides and repellent products should always be used
with caution, avoiding direct inhalation of spray or smoke.
Note: Things like Garlic, Vitamin B and ultrasound
devices etc. do not prevent or reduce bites.
 Filariasis Filariasis
Filariasis
is a worm infestation confined mainly to the tropics and spread
from person to person by the bites of mosquitoes and other
flying insects. Many types of mosquito are involved in transmission.
The severity of the disease depends on the number of worms
present.
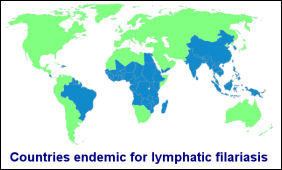
Filariasis affects an estimated 120
million persons in tropical areas of the world, including
sub-Saharan Africa, Egypt, southern Asia, the western Pacific
islands, the northeastern coasts of South and Central America,
and the Caribbean Islands.
The disease is caused by long thread like worms up to 50cm
in length which live under the skin and in lymphatic tissues.
The female worms release larvae that circulate in the peripheral
blood vessels and are ingested by mosquitoes; thus, infected
mosquitoes transmit the infection from person to person. Filarial
worms can live up to twenty years in humans producing larvae
that infect insects but the worms do not multiply in the body.
 Short-term
travelers to endemic areas are at low risk of contracting
filariasis but travelers who visit endemic areas for extended
periods of time and who are intensively exposed to infected
mosquitoes etc. can become infected. No vaccine is available. Short-term
travelers to endemic areas are at low risk of contracting
filariasis but travelers who visit endemic areas for extended
periods of time and who are intensively exposed to infected
mosquitoes etc. can become infected. No vaccine is available.
Protective measures involve avoidance of mosquito bites through
the use of personal protection measures.
Symptoms vary widely between individuals but severe cases
include inflammatory swelling of the arms and legs.
Some forms of the disease can cause blindness. In all cases,
drug treatment is effective if given before the disease becomes
advanced.
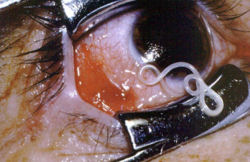
Loa loa is the filarial nematode (roundworm) species that
causes Loa loa filariasis. It is commonly known as the "eye
worm".and is one of three parasitic filarial nematodes
that cause subcutaneous filariasis in humans.
 Loa
Loa (African Eyeworm) Loa
Loa (African Eyeworm)
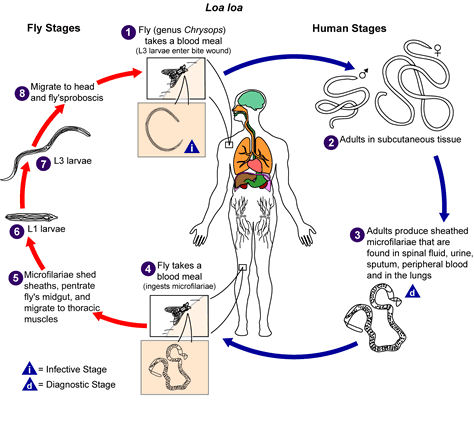
Loa loa, also known as African eye worm, is caused by the
parasitic worm Loa loa. It is transmitted through the repeated
bites of mango flies (or mangrove flies also known as deerflies
) of the genus Chrysops. The flies that transmit the parasite
breed in the rain forests of West and Central Africa. In addition
to eye worm, the infection is most commonly associated with
recurrent episodes of itchy swellings known as Calabar Swellings.
The flies that transmit Loa loa bite during the day. The infective
larvae are present in the mouth parts of the fly and enter
the wound made in the skin by the fly when it takes a blood
meal from a human.
 Once
larvae enter the human body they usually mature to adult worms
in around 5 months. Adult worms live between layers of connective
tissue under the skin. Fertilized females can produce thousands
of larvae a day. The larvae then migrate into the lymphatic
system and accumulate in the lung. Once
larvae enter the human body they usually mature to adult worms
in around 5 months. Adult worms live between layers of connective
tissue under the skin. Fertilized females can produce thousands
of larvae a day. The larvae then migrate into the lymphatic
system and accumulate in the lung.
These larvae are intermittently released into the blood stream.
It usually takes 5 to 6 months or longer after initial infection
for the larvae to be found in the bloodstream. The larvae
can survive up to one year in the human body. Adult worms
may live up to 17 years in an infected person and can continue
to release new larvae into the body for much of this time.
If a mango fly takes a blood meal from an infected human and
ingests larvae, the larvae will infect cells in its abdomen.
After 7 to 12 days the larvae mature into larvae that are
infective for humans.
 Most
people with Loa loa do not experience signs or symptoms of
infection, though persons who do not live in areas where the
parasite is found, such as travelers to the area, are more
likely to experience them. The most common manifestations
of the disease are Calabar swellings and eye worm. Most
people with Loa loa do not experience signs or symptoms of
infection, though persons who do not live in areas where the
parasite is found, such as travelers to the area, are more
likely to experience them. The most common manifestations
of the disease are Calabar swellings and eye worm.
Calabar swellings are localized, non-tender swellings usually
found on the limbs and near joints. They are associated with
itching that occurs in the area of the swelling or is generalized
to the large areas of the body.
Eye worm is the visible migration of the adult worm across
the surface of the eye. Eye worm can be accompanied by eye
congestion, itching, pain, and light sensitivity. Although
eye worm can be very distressing, it usually lasts less than
one week (often just hours) and commonly causes minimal damage
to the eye.
The main methods of diagnosis include the presence of microfilariae
in the blood, the presence of a worm in the eye, and the presence
of Calabar skin swellings.
 Treatment
of Loa loa can be difficult and should be made in consultation
with an expert in infectious diseases or tropical medicine.
The most straightforward treatment is surgical removal of
adult worms migrating under the skin or across the eye. This
can be done with local anesthesia and offers immediate relief,
though this only relieves local symptoms and does not cure
the patient of the underlying infection. Treatment
of Loa loa can be difficult and should be made in consultation
with an expert in infectious diseases or tropical medicine.
The most straightforward treatment is surgical removal of
adult worms migrating under the skin or across the eye. This
can be done with local anesthesia and offers immediate relief,
though this only relieves local symptoms and does not cure
the patient of the underlying infection.
There are two antiparasitic agents that can be used to treat
the infection and manage the symptoms; diethylcarbamazine
and albendazole. Diethylcarbamazine kills both the larvae
and the adult worms and albendazole, which kills the adult
worms.
 Diethylcarbamazine
is the preferred treatment but there is a risk of fatal brain
inflammation which can be reduced through appropriate testing
and management. In some cases, treatment is not recommended. Diethylcarbamazine
is the preferred treatment but there is a risk of fatal brain
inflammation which can be reduced through appropriate testing
and management. In some cases, treatment is not recommended.
There are no vaccines available to prevent infection with
Loa loa. Diethylcarbamazine 300mg taken once a week is effective
at preventing it in long-term travelers to affected areas.
Since the mango flies breed in muddy, shaded areas along rivers
and are attracted to smoke from wood fires, avoiding those
areas may reduce the risk of infection.
Other prevention efforts include personal protection measures
against biting insects. This includes wearing insect repellant
such as DEET on exposed skin, wearing long sleeves and long
pants during the day when deer flies bite, and wearing permethrin
treated clothing.
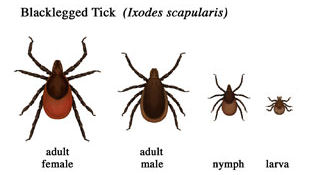
Lyme Disease
 Lyme
disease is a bacterial infection that is spread to humans
by infected ticks. Ticks are tiny arachnids found in woodland
areas that feed on the blood of mammals, including humans. Lyme
disease is a bacterial infection that is spread to humans
by infected ticks. Ticks are tiny arachnids found in woodland
areas that feed on the blood of mammals, including humans.
Ticks attach to people and animals by climbing on them when
they brush past. Ticks are commonly found in tall grass, shrubs,
and other vegetation.
Tick bites often go unnoticed and the tick can remain
feeding for several days before dropping off. The longer the
tick is in place, the higher the risk of it passing on the
infection.
The disease is characterised initially by an expanding red
rash at the site of the bite often accompanied by headache,
muscle and joint aches and fever.
The earliest and most common symptom of Lyme disease is a
pink or red circular rash that develops around the area of
the bite, three to 30 days after someone is bitten. The rash
is often described as looking like a bull’s-eye on a
dart board.
 |
There
may also be flu-like symptoms, such as tiredness, headaches
and muscle or joint pain.
If Lyme disease is left untreated, further symptoms
may develop months or even years later and can include:
-
muscle
pain
-
joint
pain and swelling of the joints
-
neurological
symptoms, such as temporary paralysis of the facial
muscles
|
Lyme disease
in its late stages can trigger symptoms similar to those of
fibromyalgia or chronic fatigue syndrome. This is known as chronic
Lyme disease. More research into this form of Lyme disease is
needed.
 A person
with Lyme disease is not contagious because the infection can
only be spread by ticks.
A person
with Lyme disease is not contagious because the infection can
only be spread by ticks.
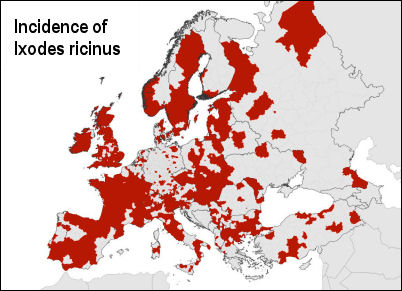
Ixodes ricinus, the castor bean tick, is a European species
of hard-bodied tick that can reach a length of 11 mm (0.43 in)
when engorged with a blood meal, and can transmit both bacterial
and viral pathogens such as the causative agents of Lyme disease
and tick-borne encephalitis.
Lyme disease occurs in temperate forested
regions of Europe (including the UK) and Asia and in the northeastern,
north central, and Pacific coastal regions of North America,
Australia, China and Japan. It is not transmitted in the tropics.
The Health Protection Agency (HPA) estimates that there are
2,000 to 3,000 cases of Lyme disease in England and Wales each
year, and that about 15%-20% of cases occur while people are
abroad.
Parts of the UK that are known to have
a high population of ticks include:
-
Exmoor
-
The
New Forest
-
The
South Downs
-
Wiltshire
and Berkshire
|
-
Thetford
Forest
-
The
Lake District
-
The
Yorkshire Moors
-
The
Scottish Highlands
|
 |
 Most
tick bites occur in late spring, early summer and during the
autumn because these are the times of year when most people
take part in outdoor activities, such as hiking and camping. Most
tick bites occur in late spring, early summer and during the
autumn because these are the times of year when most people
take part in outdoor activities, such as hiking and camping.
Prolonged
exposure to tick habitats increase the risk of Lyme disease
and should be avoided if possible. If exposure to tick habitats
cannot be avoided, the application of repellents to skin and
clothing, as well as regular daily checks for any attached
ticks, can reduce the risk of infection. Prompt removal of
any attached ticks will help prevent infection.
 Repellents
containing DEET have been found to be useful but if an embedded
tick is discovered, slowly pulling it out with tweezers is
the best method of removal and the affected person should
remain alert to the development of any symptoms. If a rash
appears at the site of attachment, immediate medical attention
should be sought. Lyme disease is effectively treated with
oral penicillin or tetracyclines. Repellents
containing DEET have been found to be useful but if an embedded
tick is discovered, slowly pulling it out with tweezers is
the best method of removal and the affected person should
remain alert to the development of any symptoms. If a rash
appears at the site of attachment, immediate medical attention
should be sought. Lyme disease is effectively treated with
oral penicillin or tetracyclines.
A safe and efficacious vaccine was, until recently (Feb 2002),
available for protection from Lyme disease. However, production
of the vaccine was discontinued by the manufacturer because
of low demand and is no longer commercially available.
The best way to prevent getting Lyme disease is to be aware
of the risks when you visit areas where ticks are likely to
be found and to take sensible precautions.
When travelling
to other European countries or to North America, where the
infection occurs more frequently than in the UK, you should
also be aware of the risks.
You can
reduce the risk of infection by:
-
being
aware of ticks and the areas where they usually live
-
wearing
appropriate clothing in tick-infested areas (a long-sleeve
shirt and trousers tucked into your socks)
-
wearing
light-coloured fabrics that may help you spot a tick on
your clothes
-
using
insect repellents
-
inspecting
your skin for ticks, particularly at the end of the day,
including your head, neck and skin folds (armpits, groin,
and waistband)
-
checking
your children’s head and neck areas, including their
scalp
-
making
sure that ticks are not brought home on your clothes
-
checking
that pets do not bring ticks into your home in their fur

Oral
antibiotics are recommended for treating early, mid- and late-stage
Lyme disease. Most people will require a two- to four-week
course depending on the stage of the condition. It is very
important that the course of antibiotics is completed to ensure
that all the bacteria are destroyed.
If
symptoms are particularly severe and include arthritis or
neurological conditions, intravenous antibiotics may be used.
Most people with mid or late stage Lyme disease will require
a course of intravenous antibiotics.
 Leishmaniasis Leishmaniasis
Leishmaniasis is a widespread parasitic disease caused
by single celled organisms called leishmania which are transmitted
by the bite of an infected sandfly (phlebotomus).
Sandflies are also responsible for inflicting itchy bites on
people. The bites can be treated with antihistamines.
The disease occurs in three forms, cutaneous leishmaniasis,
mucocutaneous leishmaniasis, and visceral leishmaniasis, each
of which varies in incidence and severity. The three predominant
forms of leishmaniasis can affect the skin, mucosa, and/or internal
organs resulting in severe disfigurement, disability, or death.
Leishmaniasis is endemic in 88 countries across four
continents with around 350 million people currently at risk
of infection. Each year it is estimated that 1.6 million new
infections occur as well as 47,000 deaths.
Cutaneous: the infection is restricted to the skin at
the site of the bite where it manifests as skin nodules on the
face, arms and legs which may form ulcers. The disease is normally
self limiting but can leave the victim with disfiguring scars.
The disease is found throughout North Africa, the Middle East,
Asiatic Russia, Iran and tourist resorts around the Mediterranean.
The disease is often called "Oriental Sore".
 Mucocutaneous:
For unknown reasons, certain species of Leishmania parasites
migrate beyond the site of initial sandfly bite to cause the
more extensive disease; mucocutaneous leishmaniasis. Mucocutaneous
disease occurs when parasites migrate to mucosal surfaces, generally
of the nose or mouth. Mucocutaneous:
For unknown reasons, certain species of Leishmania parasites
migrate beyond the site of initial sandfly bite to cause the
more extensive disease; mucocutaneous leishmaniasis. Mucocutaneous
disease occurs when parasites migrate to mucosal surfaces, generally
of the nose or mouth.
As with cutaneous lesions, parasites replicate in the tissues
causing damage. However, unlike the cutaneous form of the disease,
mucocutaneous lesions are not self-limiting and can result in
permanent damage or loss of the nose, soft palate, or lips.
Mucocutaneous disease is the least common form of leishmaniasis
and is primarily limited to South America.
Visceral: (Kala Azar) in this instance the parasites
invade the liver, spleen and bone marrow causing serious illness,
which, if untreated can lead to death. The main problem being
failure in diagnosis. It is sometimes misdiagnosed as leukaemia
or lymphoma due to enlargement of the spleen, anaemia and weight
loss. It occurs in the same regions as the cutaneous form but
is more widespread in parts of Africa, India and South America.
Children are especially at risk.
Most cases of leishmaniasis respond well to treatment with an
antimony drug (sodium stibogluconate) if diagnosed early enough.

 Sleeping
Sickness Sleeping
Sickness
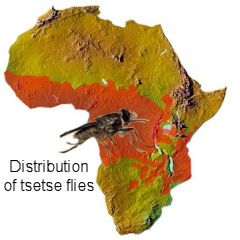
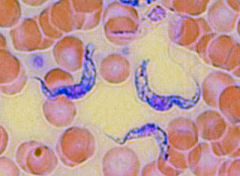
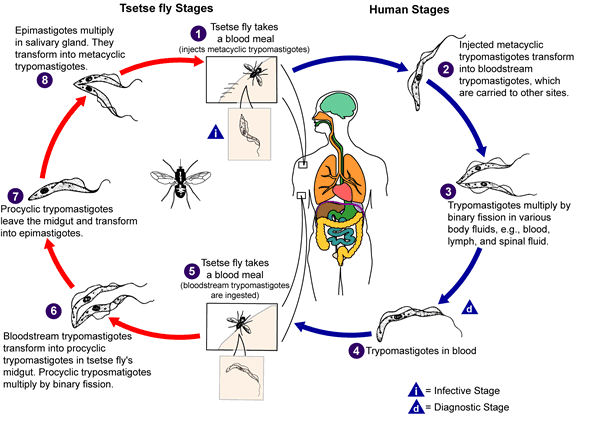
African Trypanosomiasis, also known as "sleeping
sickness," is caused by microscopic parasites called
trypanosomes. It is transmitted by the bites of infected tsetse
flies and is confined to areas of tropical Africa.
Sleeping Sickness has been a serious public health problem
in some regions of sub-Saharan Africa with about 10,000 new
cases each year being reported and it is believed that many
cases go undiagnosed and unreported.
Sleeping sickness is curable with medication, but is fatal
if left untreated.
There are two subspecies of the parasite Trypanosoma brucei
that cause the disease in humans.They are found in different
regions of Africa (East & West African Sleeping Sickness).
At present, there is no overlap in their geographic distribution.
 East
African sleeping sickness is found in focal areas of eastern
and southeastern Africa. Over 95% of the cases of human infection
occur in Tanzania, Uganda, Malawi, and Zambia. Animals are
the primary reservoir of infection. Cattle have been implicated
in the spread of the disease to new areas and in local outbreaks.
A wild animal reservoir is thought to be responsible for sporadic
transmission to hunters and visitors to game parks. Infection
of international travelers is rare, but it occasionally occurs.
Most cases of sleeping sickness in travelers are amongst those
who went on safari in East Africa. East
African sleeping sickness is found in focal areas of eastern
and southeastern Africa. Over 95% of the cases of human infection
occur in Tanzania, Uganda, Malawi, and Zambia. Animals are
the primary reservoir of infection. Cattle have been implicated
in the spread of the disease to new areas and in local outbreaks.
A wild animal reservoir is thought to be responsible for sporadic
transmission to hunters and visitors to game parks. Infection
of international travelers is rare, but it occasionally occurs.
Most cases of sleeping sickness in travelers are amongst those
who went on safari in East Africa.
West African sleeping sickness is found predominantly
in central Africa and in limited areas of West Africa. Most
of the sleeping sickness in Africa is caused by this form
of the parasite. Over 95% of the cases of human infection
are found in Democratic Republic of Congo, Angola, Sudan,
Central African Republic, Chad, and northern Uganda.
Humans are the important reservoir of infection, although
the parasite can sometimes be found in domestic animals (e.g.,
pigs, dogs, goats). Imported infection by returning travellers
is extremely rare, and most cases have occurred in African
nationals who have immigrated rather than in returning travelers.
 Both
forms of sleeping sickness are transmitted by the bite of
the tsetse fly (Glossina species). Both male and female flies
can transmit the infection. Both
forms of sleeping sickness are transmitted by the bite of
the tsetse fly (Glossina species). Both male and female flies
can transmit the infection.
Tsetse flies breed alongside rivers and transmit the disease
between wild animals, cattle and humans. It is also responsible
for deaths amongst livestock and is therefore of economic
significance. Epidemics usually occur after outbreaks of social
or political turmoil.
East African sleeping sickness progresses rapidly. The first
sign of the illness is a boil-like swelling which arises five
or more days at the site of the bite (any sooner is probably
an allergic reaction).
Fever follows within two or three weeks along with headache,
muscle and joint aches, and enlarged lymph nodes. Sometimes
there is a rash. After a few weeks of infection, if left untreated
the parasite invades the central nervous system and eventually
causes mental deterioration and other neurologic problems
including the characteristic daytime drowsiness. Death ensues
usually within months.
 West
African sleeping sickness progresses more slowly. At first,
there may be only mild symptoms. Infected persons may have
intermittent fevers, headaches, muscle and joint aches, and
malaise. Itching of the skin and swollen lymph nodes. Weight
loss is common. West
African sleeping sickness progresses more slowly. At first,
there may be only mild symptoms. Infected persons may have
intermittent fevers, headaches, muscle and joint aches, and
malaise. Itching of the skin and swollen lymph nodes. Weight
loss is common.
 Usually,
after one to two years, there is evidence of central nervous
system involvement, with personality changes, daytime sleepiness
with nighttime sleep disturbance, and progressive confusion.
Other neurologic signs, such as partial paralysis or problems
with balance or walking may occur, as well as hormonal imbalances.
The course of untreated infection rarely lasts longer than
six or seven years and more often kills in about three years. Usually,
after one to two years, there is evidence of central nervous
system involvement, with personality changes, daytime sleepiness
with nighttime sleep disturbance, and progressive confusion.
Other neurologic signs, such as partial paralysis or problems
with balance or walking may occur, as well as hormonal imbalances.
The course of untreated infection rarely lasts longer than
six or seven years and more often kills in about three years.
Due to the unfamiliarity of the disease it can remain undiagnosed
for some time. Travellers who become unwell after returning
home from an endemic area must inform their doctor of their
itinerary.
People on wildlife safaris are most at risk. The flies are
less attracted to persons on foot than on horseback and then
they are more likely to attack the horse than the rider. They
will even follow vehicles travelling slowly through infested
areas so windows should be kept closed and any insects that
enter should be killed with a knock down insecticide spray.
Most bites that occur on the African savannah are quite painful,
and travellers often recall the bite. Travellers to urban
areas are not at risk.
There is no vaccine available and prophylactic drugs are not
recommended since they mask symptoms. Prevention depends largely
on avoidance of bites. Effective drug treatment is hazardous
and highly specialised.
Chagas Disease
 Also
known as American Trypanosomiasis, Chagas is a potentially
serious disease also caused by trypanosomes which are endemic
to South and Central America and is spread through contact
with the feces of an infected triatomine bug alsoi known as
assassin bugs or kissing bugs (a blood-sucking insect that
feeds on humans and animals). Also
known as American Trypanosomiasis, Chagas is a potentially
serious disease also caused by trypanosomes which are endemic
to South and Central America and is spread through contact
with the feces of an infected triatomine bug alsoi known as
assassin bugs or kissing bugs (a blood-sucking insect that
feeds on humans and animals).
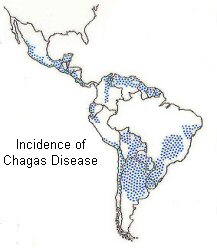
Chagas disease is endemic throughout much of Mexico, Central
America, and South America where an estimated 8 to 11 million
people are infected. The triatomine bug thrives under poor
housing conditions (for example, mud walls, thatched roofs),
so in endemic countries, people living in rural areas are
at greatest risk for acquiring infection. Public health efforts
aimed at preventing transmission have decreased the number
of newly infected people and completely halted vectorborne
transmission in some areas.
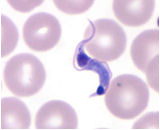
American trypanosomiasis is caused by the protozoan parasite,
Trypanosoma cruzi.
 The
disease is present in most rural areas particularly where
there is a human presence. This is because the bugs that spread
the disease live in the walls of mud huts where they venture
out, only at night to feed. The
disease is present in most rural areas particularly where
there is a human presence. This is because the bugs that spread
the disease live in the walls of mud huts where they venture
out, only at night to feed.
Travellers to these areas are most at risk but avoidance is
straightforward. True jungle areas of the Amazon are mainly
free of the disease and visitors to cities or remote jungle
ruins are not at risk.
The bugs become infected by feeding on the blood of someone
who has the disease. They then excrete infective trypanosomes
in their faeces which enter the blood of a subsequent victim
through the bite wound.
Chickens, dogs and opossums may also harbour the disease.
 Chagas
disease has an acute and a chronic phase. If untreated, infection
is lifelong. Chagas
disease has an acute and a chronic phase. If untreated, infection
is lifelong.
Acute Chagas disease occurs immediately after infection and
may last up to a few weeks or months. During this time parasites
may be found in the circulating blood. Infection may be mild
or asymptomatic. There may be fever or swelling around the
site of inoculation. Rarely, acute infection may result in
severe inflammation of the heart muscle or the brain and lining
around the brain.
Following
the acute phase, most infected people enter into a prolonged
(chronic) asymptomatic form of disease during which few or
no parasites are found in the blood. During this time, most
people are unaware of their infection. Many people may remain
asymptomatic for life and never develop Chagas-related symptoms.
However, an estimated 20% to 30% of infected people will develop
debilitating and sometimes life-threatening medical problems
over the course of their lives.
Symptoms include swelling around the site of the bite followed
by enlargement of the lymph glands and fever. Long term symptoms
include damage to the heart causing sudden death and paralysis
of the gut causing difficulty in swallowing and severe constipation.
 The
risk of acquiring Chagas disease while traveling is considered
to be extremely low. Travellers could be at risk of Chagas
disease if staying in poor-quality housing in endemic areas. The
risk of acquiring Chagas disease while traveling is considered
to be extremely low. Travellers could be at risk of Chagas
disease if staying in poor-quality housing in endemic areas.
Chagas disease could be acquired through blood transfusion
in areas with poor screening or by consuming contaminated
food or beverages.
 There
is no vaccine or preventative drug treatment available and
treatment of the disease is difficult since no drug is currently
able to kill the parasites without harming the host. Clinicians
should consult with an infectious disease or tropical medicine
specialist to diagnose and treat Chagas disease. There
is no vaccine or preventative drug treatment available and
treatment of the disease is difficult since no drug is currently
able to kill the parasites without harming the host. Clinicians
should consult with an infectious disease or tropical medicine
specialist to diagnose and treat Chagas disease.
Antitrypanosomal drug treatment is usually recommended for
acute and chronic Trypanosoma cruzi infection based
on recent data suggesting that a course of antitrypanosomal
treatment delays progression of cardiomyopathy and decreases
mortality.
Avoidance of the bites is the best strategy. When travelling
through an endemic region try not to sleep in adobe huts where
the locals sleep, keep away from walls when sleeping and use
mosquito nets. Spraying the insides of rooms with an insecticide
spray is also a good idea.
Travelers who cannot avoid camping, sleeping outdoors, or
sleeping in poorly constructed houses in endemic areas should
use insecticide-impregnated bed nets and tuck in the edges
to provide a physical barrier to the vectors.
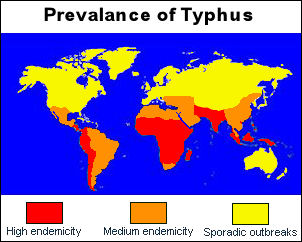
Typhus
 There
are several varieties of typhus all of which cause fever,
severe headache and a skin rash (spotted fever) and the severity
of the illness varies greatly among the different types. In
the past, outbreaks of typhus fever have been responsible
for thousands of deaths. There
are several varieties of typhus all of which cause fever,
severe headache and a skin rash (spotted fever) and the severity
of the illness varies greatly among the different types. In
the past, outbreaks of typhus fever have been responsible
for thousands of deaths.
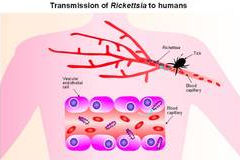
All forms of typhus fever are caused by tiny organisms called
rickettsiae which are passed on to humans by various types
of insects including lice (epidemic), fleas (endemic), mites
(scrub) and ticks. Ricketsial illness exists world-wide
 All
age groups are at risk of rickettsial infections during travel
to endemic areas. Transmission is increased during outdoor
activities in the spring and summer months when ticks and
fleas are most active. However, infection can occur throughout
the year. All
age groups are at risk of rickettsial infections during travel
to endemic areas. Transmission is increased during outdoor
activities in the spring and summer months when ticks and
fleas are most active. However, infection can occur throughout
the year.
Because of the five to fourteen day incubation period for
most rickettsial diseases, tourists may not necessarily experience
symptoms during their trip, and onset may coincide with their
return home or develop within a week after returning. Epidemic
typhus is only likely to affect volunteer workers who come
into close contact with locals.
Rickettsial infections among travelers include Mediterranean
spotted fever from southern Europe and Africa, Indian tick
typhus from India, Astrakhan fever from southeastern Europe
and central Africa, Israeli tick typhus from Mediterranean
countries, Thai tick typhus from Asia and Australia, Queensland
tick typhus and Australian spotted fever from eastern Australia,
tickborne lymphadenopathy from European countries, north Asian
tick typhus from China and Russia, Rocky Mountain spotted
fever and Rickettsia parkeri from the Americas, and African
tick-bite fever from Africa and the Caribbean islands.
Game hunting and traveling to southern Africa from November
through April are risk factors for African tick-bite fever
in travelers. Contact with tick-infested dogs in areas endemic
for certain rickettsiae may increase the risk of disease.
One study estimated that the risk of a traveler contracting
a rickettsiosis in southern Africa isfour to five times higher
than that of acquiring malaria.
Epidemic typhus occurs in communities and refugee populations
where body lice are prevalent. Outbreaks often occur during
the colder months when infested clothing is not laundered.
 Travelers
at most risk for epidemic typhus include those who may work
with or visit areas with large homeless populations, impoverished
areas, refugee camps, and regions that have recently experienced
war or natural disasters. Travelers
at most risk for epidemic typhus include those who may work
with or visit areas with large homeless populations, impoverished
areas, refugee camps, and regions that have recently experienced
war or natural disasters.
People who walk through tropical bush should inspect their
skin for any attached ticks and carefully remove them. There
are no vaccines available for any form of typhus.
typhus,usually manifests with a sudden onset of headache,
chills, fever, and general pains. On the third to fifth day
a rash and toxemia develpos. About ten days after being bitten,
an infected person experiences headache, loss of appetite,
malaise, and a rapid rise in temperature with fever, chills,
marked prostration, and nausea. Four to six days after onset,
a characteristic rash appears over most of the body; the sick
person is flushed, and the eyes are bleary.
The severity of the illness depends on the variety of typhus.
The disease can be fatal but responds well to antibiotic therapy
using tetracyclines if given early enough.
 Rocky
Mountain Spotted Fever Rocky
Mountain Spotted Fever
is a
tickborne disease caused by Rickettsia rickettsii.
This organism is a cause of the potentially fatal human illness
in North and South America, and is transmitted to humans by
the bite of infected ticks. In the United States, these include
the American dog tick, Rocky Mountain wood tick, and brown
dog tick.
Typical symptoms include: fever, headache, abdominal pain,
vomiting, and muscle pain. A rash may also develop, but is
often absent in the first few days, and in some patients,
never develops. Rocky Mountain spotted fever can be a severe
or even fatal illness if not treated in the first few days
of symptoms.
Doxycycline is the first line treatment for adults and children
of all ages, and is most effective if started before the fifth
day of symptoms. The initial diagnosis is made based on clinical
signs and symptoms, and medical history, and can later be
confirmed by using specialized laboratory tests. Rocky Mountain
Spotted Fever and other tickborne diseases can be prevented.
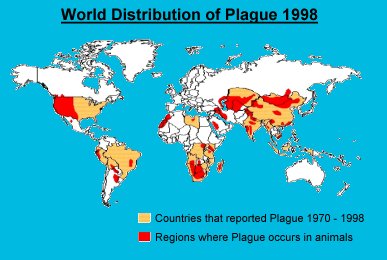
Plague
 Otherwise
known as The Black Death, this disease is one of the oldest
known and is found world-wide including the USA. In the fourteenth
century it spread across Europe and was responsible for wiping
out one third of the population. Otherwise
known as The Black Death, this disease is one of the oldest
known and is found world-wide including the USA. In the fourteenth
century it spread across Europe and was responsible for wiping
out one third of the population.
The causative organism is a bacterium (Yersinia Pestis)
and it is primarily a disease of rodents especially rats.
These bacteria are found in many areas of the world, including
the United States in rural and semi-rural areas of the western
states and is most common in the southwestern states, particularly
New Mexico, Arizona, and Colorado. Human plague occurs in
areas where the bacteria are present in wild rodent populations.
The risks are generally highest in rural and semi-rural areas,
including homes that provide food and shelter for various
ground squirrels, chipmunks and wood rats, or other areas
where you may encounter rodents.
 People
most commonly acquire plague when they are bitten by a flea
that is infected with the plague bacteria. People can also
become infected from direct contact with infected tissues
or fluids while handling an animal that is sick with or that
has died from plague. Finally, people can become infected
from inhaling respiratory droplets after close contact with
cats and humans with pneumonic plague. People
most commonly acquire plague when they are bitten by a flea
that is infected with the plague bacteria. People can also
become infected from direct contact with infected tissues
or fluids while handling an animal that is sick with or that
has died from plague. Finally, people can become infected
from inhaling respiratory droplets after close contact with
cats and humans with pneumonic plague.
Rat fleas (Xenopsylla cheopis) become infected by feeding
on the blood of an infected rodent. The infection is then
spread to humans by the bite of the rat flea. When the rodents
die the fleas go in search of a new host. They can then transmit
the disease to humans who become their hosts.
The disease manifests itself in three forms; bubonic plague,
septicaemic plague and pneumonic plague:-
-
 Bubonic
plague:
About seven days after exposure patients develop sudden
onset of fever, headache, chills, and weakness and one
or more swollen, tender and painful lymph nodes (called
buboes). This form is usually the result of an infected
flea bite. The bacteria multiply in the lymph node closest
to where the bacteria entered the human body. If the patient
is not treated with appropriate antibiotics, the bacteria
can spread to other parts of the body. Bubonic
plague:
About seven days after exposure patients develop sudden
onset of fever, headache, chills, and weakness and one
or more swollen, tender and painful lymph nodes (called
buboes). This form is usually the result of an infected
flea bite. The bacteria multiply in the lymph node closest
to where the bacteria entered the human body. If the patient
is not treated with appropriate antibiotics, the bacteria
can spread to other parts of the body.
-
Septicaemic
plague: Patients develop fever, chills, extreme weakness,
abdominal pain, shock, and possibly bleeding into the
skin and other organs. Skin and other tissues may turn
black and die, especially on fingers, toes, and the nose.
Septicemic plague can occur as the first symptoms of plague,
or may develop from untreated bubonic plague. This form
results from bites of infected fleas or from handling
an infected animal.
- Pneumonic
plague: Patients develop fever, headache, weakness,
and a rapidly developing pneumonia with shortness of breath,
chest pain, cough, and sometimes bloody or watery mucous.
Pneumonic plague may develop from inhaling infectious droplets
or from untreated bubonic or septicemic plague that spreads
to the lungs. The pneumonia may cause respiratory failure
and shock. Pneumonic plague is the most serious form of
the disease and is the only form of plague that can be spread
from person to person (by infectious droplets).
 Untreated,
the disease can spread rapidly throughout the body via the
lymphatic system. However, plague can now be successfully
treated with antibiotics. Untreated,
the disease can spread rapidly throughout the body via the
lymphatic system. However, plague can now be successfully
treated with antibiotics.
In the pre-antibiotic era, mortality among those infected
with plague was around 66%. Antibiotics greatly reduced mortality,
and nowadays overall mortality has decreased to 11%.
Plague can still be fatal despite effective antibiotics,
though it is lower for bubonic plague cases than for septicaemic
or pneumonic plague cases.
Once a patient is diagnosed with suspected plague they should
be hospitalized and, in the case of pneumonic plague, medically
isolated.
Laboratory tests should be done, including blood cultures
for plague bacteria and microscopic examination of lymph node,
blood, and sputum samples.
Antibiotic treatment should begin as soon as possible after
laboratory specimens are taken. To prevent a high risk of
death in patients with pneumonic plague, antibiotics should
be given as soon as possible, preferably within 24 hours of
the first symptoms.
|