|
What
is decompression sickness?
 Decompression
sickness, also called the bends, is caused by nitrogen
bubbles forming in the bloodstream and tissues of the
body. The bubbles occur if you move from deep water
towards the surface (where the surrounding pressure
is lower) in too short a space of time. Decompression
sickness, also called the bends, is caused by nitrogen
bubbles forming in the bloodstream and tissues of the
body. The bubbles occur if you move from deep water
towards the surface (where the surrounding pressure
is lower) in too short a space of time.
Symptoms
occur soon after the dive has finished and, in the
most serious cases, it can lead to unconsciousness or
death.
If
you suspect decompression sickness, initiate first aid
immediately and summon assistance from a specialist
in divers' medicine.
Treatment is 100 per cent oxygen on site and during
transportation, followed by treatment in a decompression
chamber.
|
What
if you or your buddy
have symptoms?
|
- If
the diver becomes unconscious, give first aid.
- Summon
the emergency services immediately.
- Administer
pure (100%) oxygen if available.
- Avoid
over-exertion. Lie the victim down with their
feet slightly raised.
- Drink
plenty of liquid.
- Any
unusual condition after a dive should be considered
as decompression sickness until proven otherwise.
So always get medical help.
|
What
are the symptoms?
The
symptoms of decompression sickness vary because the
nitrogen bubbles can form in different parts of the
body.
The
diver may complain of headache or vertigo, unusual tiredness
or fatigue. He or she may have a rash, pain in one or
more joints, tingling in the arms or legs, muscular
weakness or paralysis. Less often, breathing difficulties,
shock, unconsciousness or death may be seen.
The
symptoms generally appear in a relatively short period
after completing the dive. Almost 50 per cent of divers
develop symptoms within the first hour after the dive,
90 per cent within six hours and 98 per cent within
the first 24 hours.
In
practice this means symptoms that appear more than 24
hours after the dive are probably not decompression
sickness.
An exception is if the diver has travelled in an aircraft
or has been travelling in the mountains. Under these
circumstances, low pressure can still trigger decompression
sickness more than 24 hours after the last dive. As
a result, it is wise not to fly within 24 hours of a
deep dive.
Why does it happen?

Nitrogen makes up 79 per cent of the air we breathe
(in the air around us and in our diving bottles). During
a dive, large amounts of nitrogen are taken into the
body's tissues. This is because the diver is breathing
air at a higher pressure than if they were at the surface.
The
quantities of dissolved nitrogen depend on the depth
and duration of the dive. The deeper and longer the
dive, the more nitrogen is taken up by the body. This
does not present a problem as long as the diver remains
under pressure.
As the diver begins to ascend to the surface, the surrounding
pressure falls, and nitrogen is released from the body
via the lungs when the diver breathes out.
If the rate of ascent exceeds that at which nitrogen
can be released, it forms bubbles in the blood and tissues
(similar to opening a bottle of fizzy drink too quickly).
To minimise the risk of bubbles forming and divers developing
decompression sickness, various tables have been drawn
up that show the relationship between a given depth
of water and the time a diver can stay down.
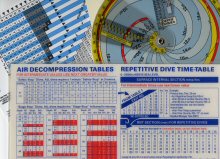
Decompression Tables |
In
addition, divers are advised to make a safety stop every
5m, and not to ascend at a pace of more than 10m a minute.
If the dive has been deep or of long duration, it may
be necessary to stop one or more times on the way up,
making so-called decompression stops.
However,
following the advice of the tables is no guarantee of
avoiding decompression sickness. This is because the
risk of developing decompression sickness is not only
determined by the depth and length of the dive, but
also by any safety/decompression stops. Factors such
as cold, current, exertion and lack of fluid also play
a part.
Personal characteristics such as age, sex, percentage
of body fat and physical condition must also be considered.
Women are more at risk of decompression sickness than
men. Similarly, the risk becomes greater the older the
diver and also depends on the level of physical fitness.
How
is it diagnosed?
 In
most cases, the diving history (ie information on the
number of dives, diving depth, dive time, rate of ascent
and decompressions) as well as information on contributory
factors such as cold, current, work and the diver's
physical condition will give some indication as to whether
it could be decompression sickness.
In
most cases, the diving history (ie information on the
number of dives, diving depth, dive time, rate of ascent
and decompressions) as well as information on contributory
factors such as cold, current, work and the diver's
physical condition will give some indication as to whether
it could be decompression sickness.
After
a thorough examination, which includes investigating
balance, coordination, sense of touch, reflexes and
muscular strength, the doctor can build up a complete
picture to evaluate whether decompression sickness is
likely.
The
doctor will also decide if the diver requires treatment
in a decompression chamber (also called a hyperbaric
or recompression chamber).
What
measures can be taken to avoid decompression sickness?
 Dive
within the limits set out in the diving tables. Dive
within the limits set out in the diving tables.- Keep
your rate of ascent to a maximum 10m/min.
- Don't
plan any dives that need a decompression stop in the
water.
- Make
a 3 minute safety stop at a depth of 5m, (or 1 minute
at 3m).
- Don't
dive more than three times in one day.
- If
you plan more than one dive in one day, start by making
the deepest dive first.
- If
you are diving for several days in a row, have a dive-free
day after two to three days.
- Don't
do any hard work before or after diving.
- Drink
lots of liquid before diving. Lack of fluid due to
heat or excess alcohol is dangerous.
- Make
sure you are in good physical condition and well rested.
Have regular medical checkups.
- Make
sure there is an interval of at least 24 hours between
diving and travel by air or climbing up mountains.
If you have had decompression treatment, the recommended
interval before the next dive is at least 48 hours.
Recovery
after decompression sickness
 Mild
forms of decompression sickness can resolve themselves
without treatment or by breathing 100 per cent oxygen
at the site of the accident. Mild
forms of decompression sickness can resolve themselves
without treatment or by breathing 100 per cent oxygen
at the site of the accident.
However, if there is any suspicion of decompression
sickness, the diver must be examined by a doctor. This
is because although it might not seem serious at the
time, the condition may deteriorate.
If the diver receives treatment at an early stage, the
chances of avoiding permanent injury are good. The longer
that treatment is delayed, the greater the risk of serious
consequences.
You should take a rest from diving after treatment for
decompression sickness. The length of this rest depends
on the severity of the decompression sickness and the
effects of treatment, and should be discussed with a
specialist in divers' medicine.
 How
is decompression sickness treated? How
is decompression sickness treated?
There
is no medicine that is used as a matter of routine in
treating decompression sickness.
At the dive site and during transport:
- Administer
100 % oxygen.
- Give
diver plenty of fluids if conscious.
- Give
first aid if appropriate.
- Prevent
the casualty from exerting himself or getting cold.
 In
hospital and specialised centres: In
hospital and specialised centres:
A decompression chamber is a steel tank that can
be pressurised.
There are decompression chambers in various places in
the UK - some of these are situated at naval centres.
The pressure in a decompression chamber is increased
by closing the doors and pumping air in.
During treatment for decompression sickness, pressure
is increased to correspond to the pressure found 18m
under water. In some cases, the pressure in the chamber
is set at 50m.
The casualty breathes pure oxygen through a mask, which
improves exhalation of nitrogen.
 At
depths in excess of 18m, and also after adequate intervals,
the mask can be removed in the chamber. Pressure in
the chamber is reduced gradually until the diver reaches
surface pressure again. At
depths in excess of 18m, and also after adequate intervals,
the mask can be removed in the chamber. Pressure in
the chamber is reduced gradually until the diver reaches
surface pressure again.
Treatment typically lasts between five and six hours.
Throughout treatment a specially trained helper stays
with the diver in the chamber. The diver's condition
is closely monitored by further examination of coordination
and balance, sense of touch, etc.
If necessary, the diver's medical specialist can join
the diver in the chamber, but otherwise takes charge
of the treatment outside the chamber in co-operation
with the specially trained helper.
 After
treatment, the diver will be kept for 24 hours for observation
in case his condition deteriorates. After
treatment, the diver will be kept for 24 hours for observation
in case his condition deteriorates.
In most instances one course of treatment is adequate,
but occasionally several treatments may be needed.
After treatment for decompression sickness, a diver
should take a rest from diving. The length of this rest
should be discussed with a specialist in divers' medicine.

|